National Academies Address Well-Being of Youth with Special Health Care Needs
Research By: Carole Lannon, MD, MPH | Thomas Boat, MD
Post Date: November 27, 2024 | Publish Date: Nov. 27, 2024
As treatments have advanced, many children and youth with special health care needs (CYSHCN) are living long into adulthood. However, challenges and uncertainty come with these advancements, and with uncertainty comes stress. Patients, families, communities, and systems may feel the physical, emotional, social, and financial impacts of chronic caregiving.
In 2023, the National Academies of Science, Engineering, and Medicine (NASEM) convened a panel of thought-leaders and partners for conversations about how to support the well-being of CYSHCN and their families. Now, a report co-authored by Cincinnati Children’s experts has been published, summarizing the discussions and key recommendations for next steps.
The report, published Nov. 27, 2024, in Pediatrics, summarizes five presentations; three from pediatric physician-scientists, including Carole Lannon, MD, MPH from Cincinnati Children’s, and two from parent-advocates.
“The National Academy of Medicine (NAM) Section on Child Health recognizes the importance of child and parent health, both physical and emotional, for the well-being of our communities, and country. They further recognize that a growing number of children have a complex, chronic health disorder that puts them and their parents at risk for health and wellbeing. The NAM webinar outlined how providers of child health care can foster resilience, support the emotional health, and better configure their programs to reduce stress for these children and their parents,” says Tom Boat, MD, a long-time leader in pediatric medicine at Cincinnati Children’s. Boat is a member of the NAM and co-author of this report in Pediatrics.
Support for Pediatricians
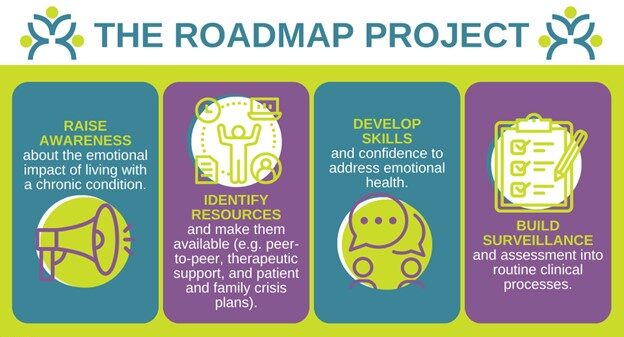
Pediatricians who care for CYSHCN must be able to screen for and address the emotional health needs of their patients and families, but many, including subspecialists and trainees, report lacking training and confidence in doing so. Individual clinicians may not know where to start. To address this gap, Lannon described the Roadmap Project which aims to promote emotional health as a routine part of excellent and equitable care for CYSHCN.
Co-designed with patients, parents, clinicians, and psychologists, Roadmap provides a number of practical resources to support clinicians: the Normalize-Ask-Pause-Connect Technique, developed by a psychologist for how to begin a conversation about emotional health; a Readiness Checklist that allows a practice to self-assess its gaps and prioritize next steps; and tools for developing a resource list, choosing a behavioral health practitioner, and billing strategies.
The report summarizes results achieved by initial pediatric Roadmap users of the American Board of Pediatrics Maintenance of Certification activity, including that staff awareness of emotional health needs increased by 34% from baseline; availability of a resource list, by 90%; provider confidence in addressing emotional health, by 79%; and availability of a crisis plan for families, by 78%.
The Power of Normalizing Emotional Impacts
The report also highlights the experience and insight shared by Diane Pickles, the mother of a son born with a complex congenital heart disease. She has worked with Roadmap since its inception.
“Healthcare providers can have a tremendous impact on patients and families by normalizing the emotional health impacts of living with complex, chronic health conditions. Asking how a patient and their family members are feeling, and letting them know that the trauma and challenges of their medical condition frequently cause stress, anxiety, and difficulty coping, is powerful,” Pickles shared.
She reminded attendees that when the emotional health impacts are not normalized, “it makes it even more difficult for patients and families to share their struggles and seek out help and support.”
The Roadmap Project, launched by the American Board of Pediatrics (ABP), is led by Lannon, who serves as senior faculty lead of the Learning Networks Program at the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s. Lannon also is the senior quality advisor for the ABP.
More information
- Learn more about the Roadmap Project
- Using Roadmap Tools with Pediatric Trainees
Carole Lannon and Tom Boat contributed to the content for this post.
| Original title: | Supporting the Well-Being of Children and Youth With Special Health Care Needs: NASEM Proceedings |
| Published in: | Pediatrics |
| Publish date: | Nov. 27, 2024 |
Research By

Identifiable gaps in health outcomes piqued my research interests. I now work with patients, families, clinicians and researchers to improve care and outcomes for children and families using learning health networks. These networks, used for improvement and research, can accelerate population health outcomes at scale.