Signal Switch Gives MDS Cells a Competitive Advantage that Supports Disease Progression
Research By: Daniel Starczynowski, PhD
Post Date: April 20, 2020 | Publish Date: April 20, 2020
A powerful clue has emerged in a long-running mystery about how the cells of myelodysplastic syndrome (MDS) manage to outcompete normal blood cells to cause a disease state that often leads to leukemia, according to a study published online April 20, 2020, in Nature Immunology.
The study includes experts from Cincinnati Children’s, the University of Cincinnati, the MD Anderson Cancer Center in Houston, and the University of California San Francisco. Daniel Starczynowski, PhD, Division of Experimental Hematology and Cancer Biology at Cincinnati Children’s, is the corresponding author.
MDS, a disease linked with certain congenital disorders and aging, is associated with a low-grade chronic state of inflammation. While this response normally would be determinantal to blood-forming hematopoietic cells, MDS hematopoietic stem cells and progenitor cells (HSPCs) avoid attack by switching a critical cell signaling pathway. The new findings identify that pathway: a non-canonical NF-κB pathway that appears to depend upon TLR-TRAF6-mediated activation of A20.
“These findings uncover the mechanistic basis for the clonal dominance of MDS HSPCs and suggest that interfering with non-canonical NF-κB signaling could prevent MDS progression,” the co-authors write.
Previous research led by Starczynowski and colleagues has established the important role of cell-intrinsic dysregulation of innate immune signaling pathways, such as TRAF6 overexpression, in the MDS disease process.
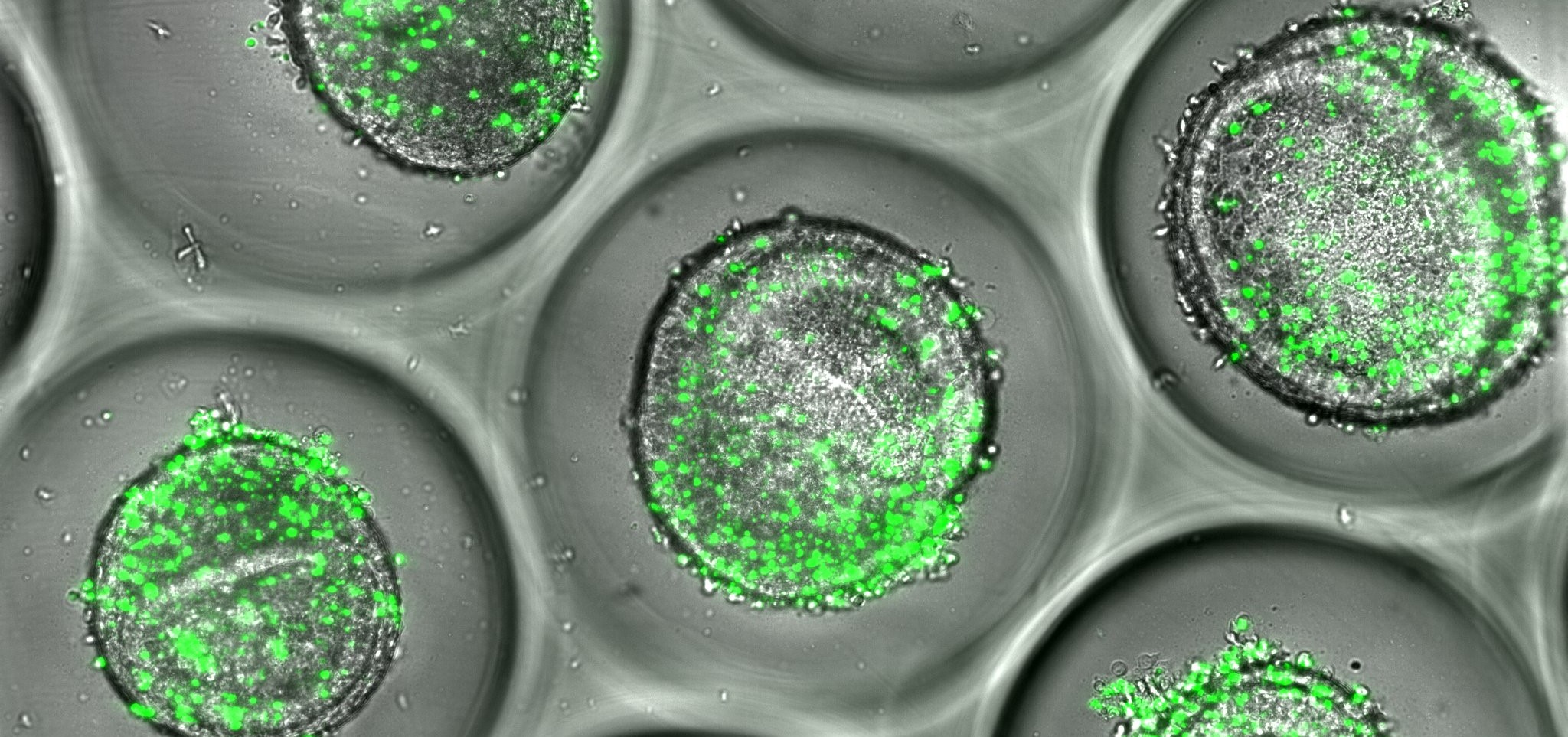
This study analyzed mouse models and human cells to determine how dysregulation of innate immune signaling pathways resulting from TRAF6 overexpression affects HSPCs during a systematic inflammatory state such as in MDS. They found that TLR-TRAF6-primed HSPCs tripled the level of A20 expression during inflammation in mouse models. A similar response was detected in human MDS cells.
A20 (also known as TNFAIP3) is a multi-faceted signaling factor gene known to play an important regulatory role in inflammation and immunity. The co-authors say that inhibiting excess A20 expression or otherwise disrupting the TLR-TRAF6 signaling pathway re-sensitizes the MDS HSPCs to low-grade inflammation and therefore could serve as potential new treatments to stop MDS from progressing into leukemia.
Starczynowski says this finding may be one of the most significant to date from his lab in more than a decade of studying MDS.
“This paper identifies the mechanistic basis for why MDS cells outcompete normal cells and contribute to disease,” he says. “The paper not only reveals important therapeutic implications on how to treat MDS, but also leads to more questions about the complexity of this disease.”
In addition to Starczynowski, co-authors from Cincinnati Children’s and UC include: first author Tomoya Muto, MD, PhD, Callum Walker, MS, Kwangmin Choi, PhD, Kathleen Hueneman, BSc, Molly Smith, Zartash Gul, MD, and Yi Zheng, PhD.
| Original title: | Adaptive response to inflammation contributes to sustained myelopoiesis and confers a competitive advantage in myelodysplastic syndrome HSCs |
| Published in: | Nature Immunology |
| Publish date: | April 20, 2020 |
Research By