Mitigating the Mental Health Burden of COVID-19
Post Date: May 22, 2022 | Publish Date:

Cincinnati Children’s applies expertise to a vital, yet long-underfunded health need
With more than 1 million deaths nationwide and counting, many millions of Americans are grieving the loss of loved ones to the pandemic. In too many cases, dying caregivers have left children behind to cope, including some kids robbed of both parents within a matter of days.
Many more young lives have been disrupted in other ways, including enduring the fear of having loved ones in intensive care and adjusting to life after adult caregivers lost jobs. Students personally coped with weeks and months of remote education, all-day masking rules, and other limitations on their activities.
Many missed out on milestone events, from birthday parties to graduations. Restrictions came down on gathering with friends, playing sports, or going to crowded places. Meanwhile, children were last in line for vaccines as the Delta variant gave way to the Omicron variant that affected many more children.
All of these disruptions occurred unevenly and unfairly from family to family across populations as endless political arguments and waves of misinformation crashed around.
“We know that the negative impacts of trauma on health are significant, and trauma comes in many forms. The impacts of the pandemic have exposed children to trauma over the past almost two years, and the chronic nature of the stressors have exacerbated existing mental health symptoms and led to the development of symptoms in others,” says Lori Stark, PhD, Director, Behavioral Medicine and Clinical Psychology. “Youth have been presenting at a higher frequency and with more intensive symptoms of anxiety and depression even as coping strategies and resources that had been available became more limited during the pandemic.”
It will likely take years to unpack all the ways the COVID-19 pandemic affected this rising generation. But here at Cincinnati Children’s—a national leader in providing and improving child mental health care—responses and research began immediately
and have carried on since.
STUDYING TELEHEALTH WHILE USING IT
Even as the hospital began shifting 80% or more of its vast outpatient services to telehealth, investigators understood that such dramatic change could affect outcomes and would require tracking and analysis. By May 2020, Cincinnati Children’s teams had begun studying the implications of remote medicine, especially on counseling services, and especially for children in low-resource families. Some preliminary data have emerged, but as the pandemic continues, so does the analysis.
Among the projects, Stephen Becker, PhD, has expanded an ongoing study of how ADHD affects emotions, sleep, academics, media use, family relations to also compare how this population fared during the pandemic. How will the surge of remote care affect outcomes?

“The experience of the COVID-19 pandemic and its consequences are likely to be particularly magnified and salient in youth with pre-existing mental health and neurodevelopmental risk, such as ADHD,” Becker says.
CAN ‘CHATBOTS’ FILL A VOID?
With necessity driving invention, years of gradual improvements in “chatbot” services based on machine learning technologies took sudden leaps in sophistication and usage.
At Cincinnati Children’s, the crisis prompted John Pestian, PhD, an expert in natural language processing and machine learning tools to team up with Michael Sorter, MD, Director, Division of Child and Adolescent Psychiatry and Jeffrey Strawn, MD, an anxiety expert in the Department of Psychiatry and Behavorial Neuroscience at the University of Cincinnati.
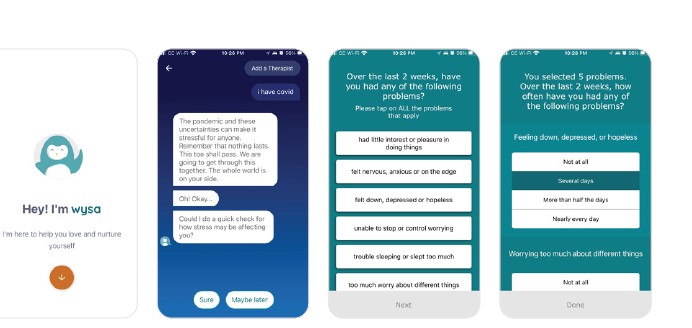
By August, 2020, they had built a working relationship with Wysa, a company that had introduced a digital behavioral health platform a few years prior in the United Kingdom and several other nations. Together, they launched an upgraded Covid Anxiety module, distributed through the Wysa app, that allowed young adults and teens to use their smartphones to chat with a “4 a.m. friend.” While not a direct counseling service, the tool invited users to explore nine exercises vetted by mental health experts.

“These self-help techniques are important because anxiety is common among the population,” says Sorter. “Unfortunately, anxiety often goes undiagnosed, and then untreated for long periods of time.”
In addition to providing comfort, the anxiety app creators fed their learnings to a team at Cambridge University that described an explosion of digital mental health solutions in a study published Feb. 10, 2021, in Frontiers in Digital Health. The report, based on data from 20 nations, documented a 7,500% increase in searches for health-apps related to the prevention of self-harm, a 176% increase for apps dedicated to the management of depression, an 86% increase in searches for mental health apps for the treatment of anxiety, and a 328% increase in searches for apps related to sleep.
“We’ve shown that it’s possible for a large number of providers to work together across borders to rapidly gather valuable insights,” said Cambridge neuroscientist Becky Inkster, DPhil, principal investigator for the study. “This could be used to set up an integrated digital system to better understand and respond to people’s mental health needs on a global scale in real-time”
SHIFTING RESEARCH FOCUS ON THE FLY
As COVID arrived, Drew Barzman, MD, Director of the Child and Adolescent Forensic Research Program at Cincinnati Children’s, had been pursuing a $7.5 million grant from the Patient-Centered Outcomes Research Institute (PCORI) to compare existing and emerging treatment options for adolescents with suicidal thoughts. By July 2021, the pandemic’s impact on mental health prompted the team to re-work the multi-center grant’s aims to build in a more extensive analysis of telehealth services.

“What we’re really wanting to take a look at is how patients are doing three months and six months out after they receive these initial services and see if there’s a clinically significant difference among the different treatment options that are available to the teens who are experiencing suicidal thoughts,” says Jennifer Combs, senior research clinical coordinator and study project manager.
To the surprise of some, the actual overall number of suicides in 2020 was 3% lower than in 2019, according to the Centers for Disease Control and Prevention’s National Center for Health Statistics. However, the numbers varied by age groups. Despite the overall decline, suicide rates increased 13% among young men ages 10 to 14 and 5% among those 25 to 34.
Data from 2021 is not yet available. Researchers are watching closely to determine how suicide and suicide ideation trends may shift as the pandemic drags on.
JUST THE BEGINNING
The full extent of the pandemic’s impact on child mental health cannot be known until the pandemic actually ends. For now, the main objectives have been to use technology to extend otherwise limited resources, to raise awareness of the soaring demand for mental health support, and to capture the data needed to assure that lessons can be learned.
“Children and adolescents were experiencing increasing mental health challenges before COVID-19, particularly depressive symptoms and suicidal ideation, and the pandemic has greatly exacerbated children’s mental health difficulties,” Stark says. “Further, the pandemic has proceeded in parallel with national attention to and reckoning with structural racism, and the mental health crisis has disproportionately impacted children from communities of color.”
The concern is so pressing that on Dec. 7, 2021, the U.S. Surgeon General released an advisory to highlight the urgent need to address the nation’s youth mental health crisis.
Looking ahead, Stark says research priorities coming out of the pandemic include identifying subpopulations at highest risk, identifying resilience factors that may be useful to promote, building and evaluating school and community based interventions to connect more youth in need to evidence-based care, and establishing expectations for telehealth and other new models of care.
On the research side, many behind-the-scenes improvements are needed to achieve these tasks, Stark says. Currently, many systems collect data separately and communicate with each other poorly. Regulatory challenges pose challenges for effective use of telemedicine. And the entire system needs more mental and behavioral health providers, especially from underrepresented populations.
“We are fortunate to have a broad continuum of services and providers that is likely unmatched in the United States,” Stark says. “Unfortunately, we also recognize that it often is not enough. We continue to see unmet needs in the community for children and their families seeking out additional services.”
Learn More About Mental Health Initiatives at Cincinnati Children’s
Transforming Mental Healthcare
$10M Investment from Cincinnati Children’s Launches Ambitious Mental Health Mission
Read More About Cincinnati Children’s COVID Response
Cincinnati Children’s Plays Central Role in COVID-19 Vaccine Clinical Trials
Contributing to COVID Knowledge
One Does Not Simply…Shut Down Science
Studying the Heart in the Storm
Pandemic Prompts Dash to Build Dashboards
Exploring Intersections Between COVID-19 and Co-Morbidities
Balancing COVID Safety and Learning Needs
Anderson Center Team RACEs to Respond to COVID
Explore the full 2021 Research Annual Report
50+ Discoveries and Innovations (Enter Research Area, click on “Featured Research”)
By-the-Numbers Section Breaks Down $270M+ in Funding
Learn About Science Careers and Student Opportunities
Find Out How You Can Support Research at Cincinnati Children’s





