$10M Investment from Cincinnati Children’s Launches Ambitious Mental Health Mission
Research By: John Pestian, PhD, MBA | Tracy Glauser, MD
Post Date: November 8, 2021 | Publish Date:

Long-range project involves analyses to be performed by one of the world’s most powerful supercomputers at Oak Ridge National Laboratories in Tennessee
Imagine a day when a mental health expert could take a look at data about a classroom of first graders and identify who is at risk for suicidal behavior as a high schooler.
Imagine a health care system that enables the people who care about those children to take action early enough to prevent such a tragedy from occurring.
That’s the ultimate goal of the bold new mental health “trajectories” project, announced Nov. 8, 2021, by leaders at Cincinnati Children’s Hospital Medical Center, one of the world’s leading pediatric research, care and training centers. It’s a massive task that will involve more than 25 leading scientists at nine different research divisions within Cincinnati Children’s as well as collaborators at the University of Cincinnati, the University of Colorado and Oak Ridge National Laboratory.

“We are seeking to show the likelihood of an individual developing serious mental illness over time. This is much like the lines of a pediatric growth chart that predict a person’s height or weight. However, these mental health trajectories are far more complex,” says Tracy Glauser, MD, Associate Director of the Cincinnati Children’s Research Foundation and one of two principal investigators for the project.
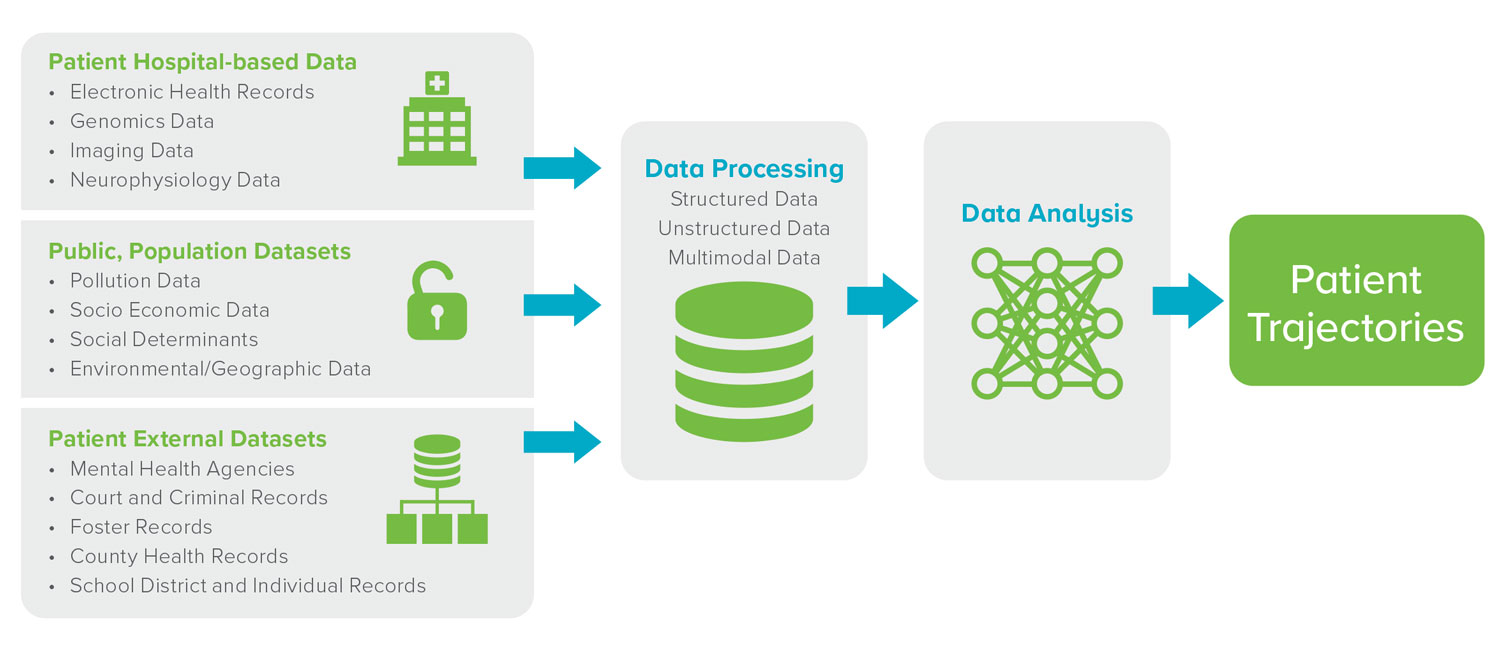
The team plans to assemble large amounts of data from many sources that investigators already know play at least some role in influencing the mental health of a growing child. Such information includes personal medical records, genomic information, environmental exposures, economic disruption, housing conditions, traumas experienced by parents, family dysfunctions, substance abuse, experiencing bullying, surviving disasters, systemic racism and more.
“Before we can cure and prevent, we have to understand the real origins of mental illness, especially the roles of biological, thought, and environment factors. Together these components are very, very complex and can only be understood with the help of the world’s most powerful computers.” says John Pestian, PhD, MBA, an expert in building neuropsychiatric artificial intelligence algorithms and co-principal investigator for the project.

One such powerful supercomputer, dubbed Summit and currently the nation’s fastest, is located at the Oak Ridge National Laboratory, a US Department of Energy national laboratory in Tennessee managed by UT-Battelle, LLC. In part to advance this work, Pestian holds dual appointments at Cincinnati Children’s and ORNL.
“We are excited to leverage ORNL’s world-class leadership computing capabilities to impact the future of pediatric mental health,” says ORNL principal investigator Greeshma Agasthya. “Improving mental health outcomes is a major challenge, and we are dedicated to using our expertise to capitalize on the wealth of information available in health records, medical notes, and medical images, while ensuring the privacy of the data.”
Anuj Kapadia, ORNL’s Section Head for Advanced Computing for Health Sciences, adds: “This collaboration, which is actively guided by clinician and pediatric mental health experts at Cincinnati Children’s, will be a step towards better mental health outcomes for our children.”
Why Mental Health?
Overall, 17.4% of U.S. children aged 2–8 years have a diagnosed mental, behavioral, or developmental disorder. That adds up to five children in every classroom of 30 students.
Childhood anxiety and depression are becoming more frequent over time. Too often, the tragic outcome of untreated and undertreated conditions is suicide—now the second leading cause of death in young people ages 10 to 24 years old. These issues can devastate families, and the impacts can span generations.
“The medical community has understood for many years that mental illnesses have been severely overlooked in terms of research priority and availability of effective treatment options. And yet, so many of the families we serve are living with the burden of seeking hard-to-obtain help for their children in need,” says Tina Cheng, MD, MPH, Chair of Pediatrics at the University of Cincinnati and Director of the Cincinnati Children’s Research Foundation.
Now, as part of its five-year strategic plan, the medical center is investing $10 million to pursue a project that could make a significance difference.
“We have been committed to improving mental health care for a number of years, including our $99 million project to expand psychiatric care capabilities at our College Hill campus. Our research faculty also has made important discoveries in the use of natural language processing to predict the risks of suicide and school violence, has developed widely-used tools used for establishing accurate doses of psychiatric medications, and many other advances,” Cheng says. “Unlike most other pediatric medical centers, we are uniquely positioned to take on the challenge of improving mental health outcomes.”
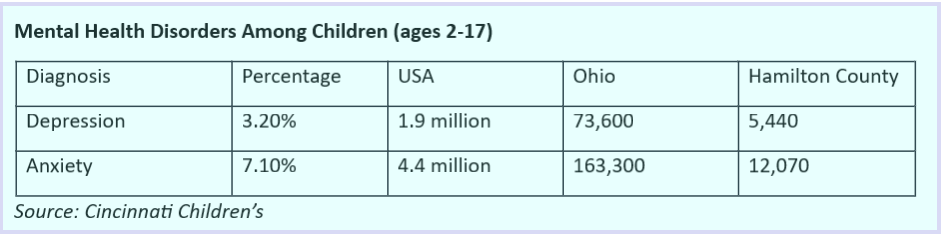
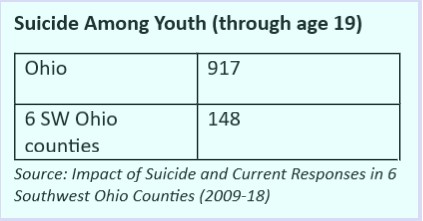
Beyond the sheer emotional impact, these mental illnesses have significant economic impacts.
“We have found studies from other researchers that estimate the economic impact of anxiety at $42 billion a year, depression at $71 billion a year and suicidal Ideation at $93.5 billion a year,” Pestian says.
What will the project entail?
The specific aims of this protocol are to develop the optimal approach to create near real-time trajectories that provide early identification of pediatric and adolescent patients who are at risk for developing depression, anxiety, and suicidality.
The team plans to integrate and analyze a complex set of biological, thought, and environmental data collected over time. By doing so, it may be possible to identify the onset of mental illness earlier in life, which in turn increases the odds of successful therapy and a better quality of life.
Data sources include neuro-physical biomarkers gathered from test results, notes made in medical and school records, video recordings, and other family status information. Those factors would be compared with population-level statistics about income levels, access to health care, pollution exposure, climate, and much more.
“We will be training a machine learning algorithm to learn from thousands of factors pulled from numerous datasets,” Pestian says. “If one were to attempt to train this model on a standard desktop computer, it would take a decade. But the supercomputer can accelerate the computational time to less than a day.” Once trained we can make the algorithms available in the clinical setting.
Over time, with more accurate data, the more accurate the trajectories will be.
Why a supercomputer?
ORNL’s Summit supercomputer was launched in June 2018. Capable of performing 200,000 trillion calculations per second—or 200 petaflops, Summit is about 10 times more powerful than ORNL’s previous top-ranked system, Titan.
Supercomputers have long played central roles in high-energy physics, materials science, and chemistry. More recently, they have been applied to wider variety of biological applications. For example, assets at ORNL are currently working to help visualize the incredibly small structures of proteins at work in our cells, to accelerate drug discovery, to better understand cancer, and more—including several COVID-19 related projects.

When attempting to study the brain, the sheer scale of the data analysis involved can be difficult to visualize, Pestian says,
Scientists estimate that the human brain has more than 100 billion neurons. That’s close to the total number of stars in the Milky Way galaxy. Each of those neurons is networked to other neurons through as many as 40,000 synapses. Calculating the immense number of connection combinations to determine which pathways are healthy vs unhealthy is no simple task.
“We will be training a machine learning algorithm to learn from thousands of factors pulled from numerous datasets,” Pestian says. “If one were to attempt to train this model on a standard desktop computer, it would take a decade. But the supercomputer can accelerate the computational time to less than a day.”
Who will be involved?
The scientists working on the trajectories project span a wide range of disciplines. They include:
- Child and Adolescent Psychiatry: Drew Barzman, MD, Craig Erickson, MD, Ernie Pedapati, MD, Michael Sorter, MD
- Behavioral Medicine and Clinical Psychology: Bob Ammerman, PhD, Sarah Beal, PhD, Scott Powers, PhD, Lori Stark, PhD, and program manager Cynthia Zion.
- Biomedical Informatics: Bruce Aronow, PhD, Stephanie Loos, MS, Alexis Mitelpunkt, PhD, Dan Santel, PhD, Mayur Sarangdhar, PhD, Andy Spooner, MD
- Biostatistics and Epidemiology: Cole Brokamp, PhD, Jareen Meinzen-Derr, PhD, Rhonda Szczesniak, PhD
- Clinical Pharmacology: Laura Ramsey, PhD, Sander Vinks, Pharm.D, PhD General Pediatrics: Andy Beck, MD
- Adolescent Medicine’s Transgender Health Clinic: Lee Ann Conard, MD
- Asthma Research: Tesfaye Mersha, PhD
- Mayerson Center for Safe and Healthy Children: Robert Shapiro, MD
- Neonatology: Kevin Dufendach, MD
- Oak Ridge National Laboratories: Greeshma Agasthya PhD, Blair Christian PhD, Anuj Kapadia PhD, Dan Jacobson, PhD, and Heidi Hanson, PhD
- University of Cincinnati Psychiatry: Jeffrey Strawn, MD
- University of Colorado Text Mining: Kevin Cohen, PhD
Where does the work stand now?
In addition to the funding commitment announced today, an agreement has been established with the Oak Ridge center, and work has begun to prepare the data for initial analysis through the supercomputer. Much more data, and many more “runs,” will be needed before a proposed set of mental health trajectories will be complete.
“It will likely be several years before we see the results of this work applied in clinical practice,” Glauser says. “However, we believe we will be ready to publish some of our initial findings within the next six months.”
In the meantime, Cincinnati Children’s has launched a campaign to raise funds to augment its initial investment.
For more information or to make a gift, please contact Ashley Titus at 513-803-6593 or ashley.titus@cchmc.org.
Learn More
Learn more about our Mind Brain Behavior research
A Machine Learning Approach to Identifying Changes in Suicidal Language, Suicide and Life Threatening Behavior, June 2020
A Machine Learning Approach to Identifying the Thought Markers of Suicidal Subjects: A Prospective Multicenter Trial. Suicide and Life-Threatening Behavior, Feb. 2017
Suicide Note Classification Using Natural Language Processing: A Content Analysis, Biomedical Informatics Insights, Aug. 2010
Pestian Joins Oak Ridge National Laboratory as Joint Faculty
Suicide Risk Prediction from Patient Interviews





