Clinical Implementation: Accelerating Best Practices
Post Date: January 24, 2024 | Publish Date:

No matter how impressive the breakthroughs nor how carefully the clinical trials are carried out, innovations in healthcare mean little until they get put to use in day-to-day care. There’s a science to quality improvement and a level of commitment that comes with knowing there’s always a way to work more effectively, more efficiently. These teams have demonstrated novel ways to put best practices into practice.
From advancing the use of virtual reality training to preventing cardiac arrest during intensive care, clinician-scientists at Cincinnati Children’s strive to be the best at getting better

Learning to Navigate a New Care Tower Before Construction is Complete
The new critical care tower at Cincinnati Children’s boasts some impressive numbers: a $600 million investment, a 632,500-square-foot facility, and 249 new private rooms.
But one of the most critical numbers may have been 2,000. That’s how many nurses, technologists and staff needed to know how to find everything in all the new spaces and know it well enough to provide a seamless transition in the fall of 2021 when patients moved in.


Attempting to provide hands-on training tours after all the building finishes were complete would have been a time-consuming logistical nightmare. So planners turned to the emerging technology of virtual reality to pave the way.
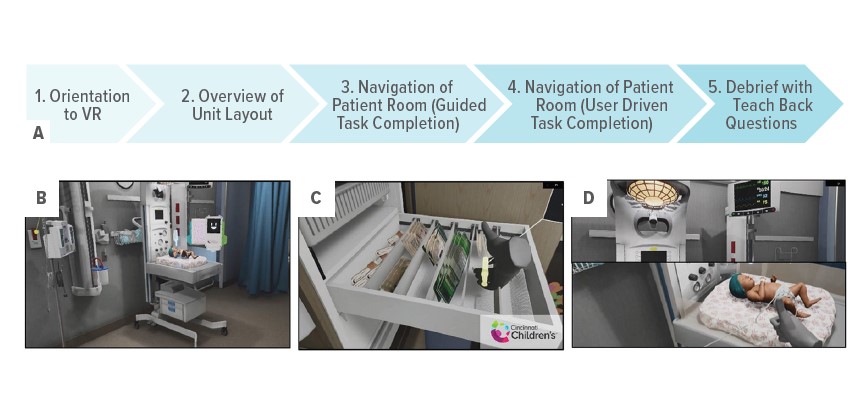
Not only did a large team of application developers, medical animators, simulation educators, clinical experts and operational leaders collaborate to design a “digital twin” of the new building, they studied how the immersive experience worked.
The team focused on building replicas of intensive care units and areas for Acute Care Cardiology and Bone Marrow Transplant. These units were prioritized because the new spaces involved the most significant changes regarding room functionality and location of resources and equipment
“Large-scale VR onboarding is feasible, tolerable, and acceptable to a diverse population of healthcare staff,” according to research led by Matthew Zackoff, MD, MEd, and senior author Ryan Moore, MD, MSc.
The investigators actually published two articles about the journey, one in The Journal of Pediatrics, and another in the journal Simulation in Healthcare.
Now virtual reality training is being used in a variety of other settings, including helping clinicians practice how to speak with families about sensitive topics like securing guns in the house when children are in crisis and the value of vaccinations against HPV, COVID and other preventable childhood diseases.
Prevention ‘Bundle’ Reduces Risk of Cardiac Arrest in ICU Care
Quality improvement experts at Cincinnati Children’s have a long history of working behind the scenes to organize networks and consortia of pediatric hospitals to share data and develop best practices to improve care outcomes.


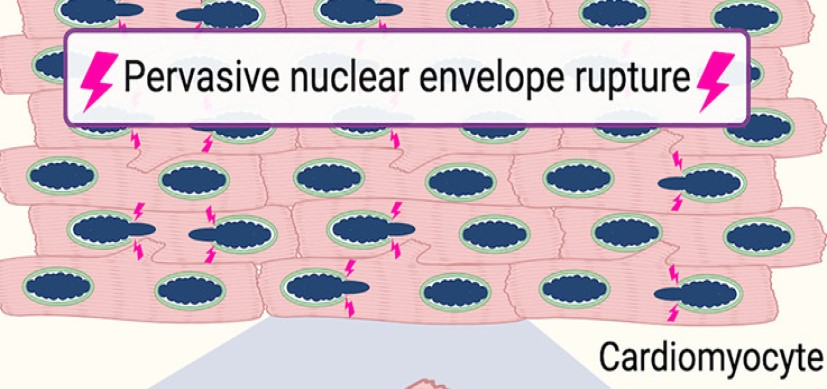
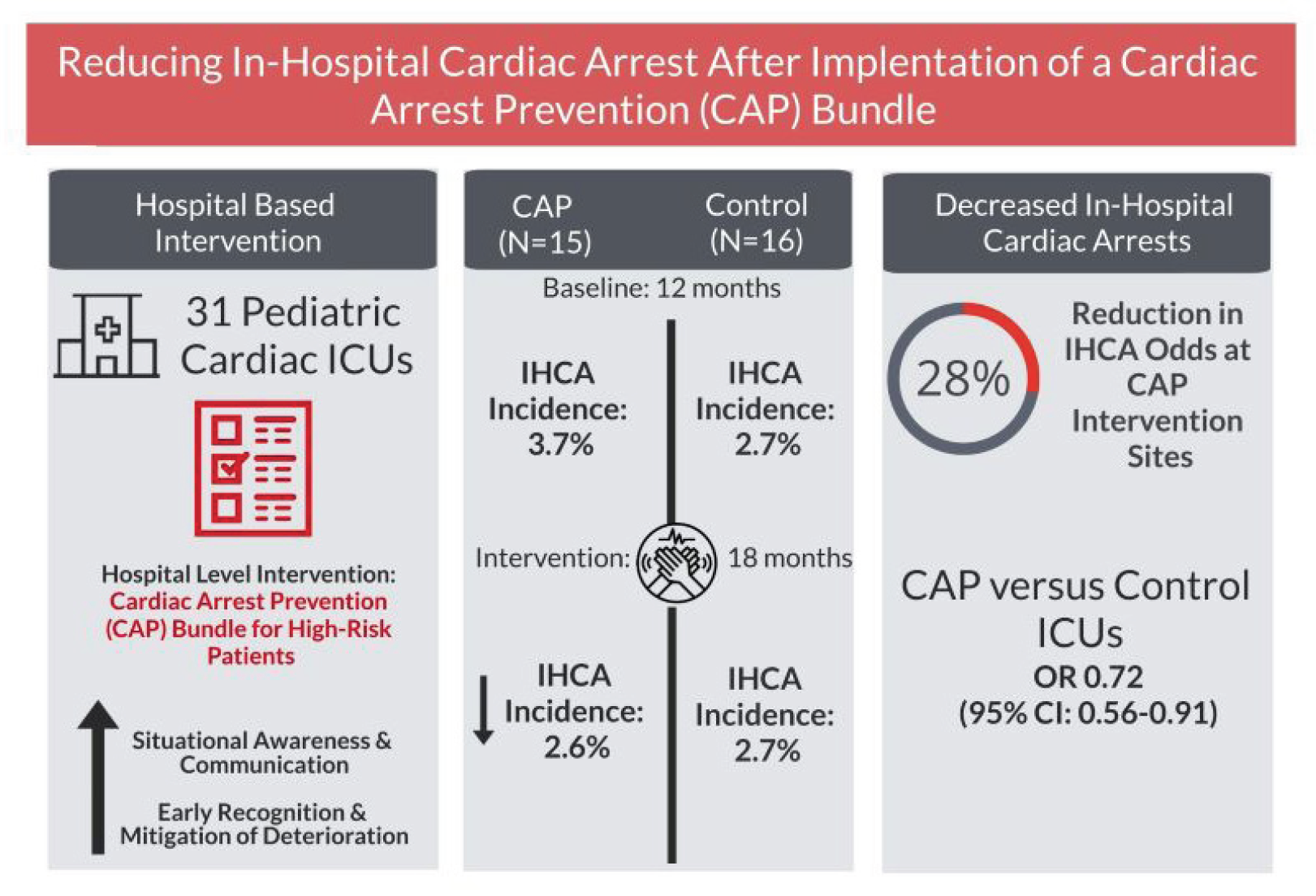
An outstanding example of this type of multicenter collaboration was published in July 2022 in JAMA Pediatrics, detailing the work of the Pediatric Cardiac Critical Consortium (PC4) to reduce cardiac arrests occurring during intensive care stays.
The participating hospitals exceeded expectations by reducing cardiac arrests by 30% after adopting a low-technology bundle of prevention practices, including safety huddles, formal code reviews and consistently storing critical emergency medications at the bedside. Project leaders were Jeffrey Alten, MD, an attending physician at Cincinnati Children’s CICU, and Michael Gaies, MD, then medical director of the Acute Care Cardiology Unit here, now co-executive director of the Heart Institute.
Read more about the prevention practices
Leading Consensus Guidelines for Pediatric Acute Kidney Injury Care
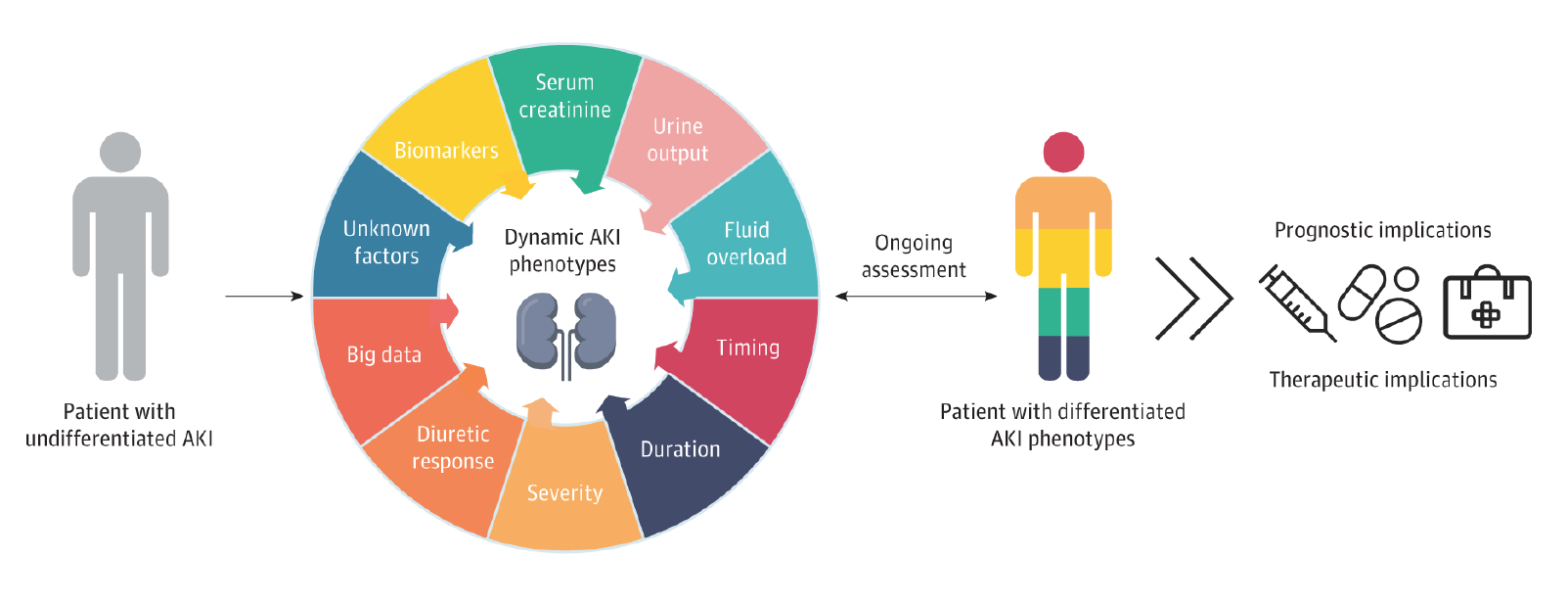
In another example of multicenter collaboration and leadership, Stuart Goldstein, MD, director of our Center for Acute Care Nephrology, served as first author for the first consensus statement focusing solely on acute kidney disease in children ever issued by the Acute Disease Quality Initiative (ADQI).

The statement, “Consensus-Based Recommendations on Priority Activities to Address Acute Kidney Injury in Children,” was published Sept. 30, 2022, in JAMA Network Open.
ADQI represents leading universities worldwide and sets new standards for the diagnosis and management of acute kidney injury and related disorders. The new statement was developed by a panel of 47 international experts at the 26th Acute Disease Quality Initiative meeting held in November 2021. It addresses issues including epidemiology, diagnostics, mechanical support, educational goals, and more.
“For a pediatric consensus document to be published in a journal with such impact and worldwide reach is unprecedented,” Goldstein says.
In addition to Goldstein’s role, Katja Gist, DO, MSc, Cardiac Intensive Care Unit (CICU) physician and co-director of the Heart Institute’s Center for Acute Care Nephrology, was pediatric ADQI co-chair for the section on AKI biomarkers.
LEND-ing a Hand in Care Training for Children with Complex Developmental Disabilities
In another specialized area of pediatric care, first authors Jennifer Smith, PsyD, BCBA-D, and Nichole Nidey, PhD, compiled learnings from more than 20 participating care centers to share the best methods for training the professionals who care for children with autism spectrum disorder (ASD) and other developmental disabilities.


The review, published in December 2022 in Pediatrics, was based on five years of data from the federally funded Leadership Education in Neurodevelopmental and related Disabilities (LEND) program. The team found that LEND trainees demonstrated improvements in knowledge, skills, and attitudes in three key competency domains.
“These findings highlight the value of LEND programs and showcase the feasibility of a national quality improvement approach,” Nidey says.
Support for a Community-Based Parent Coaching Program
Robert Shapiro, MD, is unusually well-positioned to both study and lead efforts that improve health outcomes for children who have experienced adverse childhood experiences (ACEs), such as child abuse, family dysfunction or other significant causes of stress.

Shapiro serves as director of the Mayerson Center for Safe and Healthy Children at Cincinnati Children’s and as a board member for the Beech Acres Parenting Center, the latest evolution of a long-established community organization that previously offered an orphanage and extensive foster care services.
Now, the Parent Connext® program at Beech Acres, launched in 2017, provides in-depth parent coaching and support services to help families reduce stress through strength based parenting and positive childhood experiences.
Based on data from more than 27,000 children treated at six Greater Cincinnati primary care practices, the program was linked to significantly fewer sick visits and increased the odds that children receive behavioral health referrals when needed.
“Our research highlights the potential benefit to child health from a two-generation approach, which focuses on the needs of parents and children at the same time,” Shapiro says.
Beech Acres embeds child development specialists in local pediatric practices. Parents can be referred to the program by pediatricians, or they can self-refer. Armed with impact data, next steps include work to scale-up the program to share this emerging best practice with other cities.