Scientists Find Inexpensive Ways to Reduce Cardiac Arrests in ICUs
Research By: Jeffrey Alten, MD | Michael Gaies, MD
Post Date: July 5, 2022 | Publish Date: July 5, 2022
Heart Institute: Cardiology | Top Scientific Achievement

Five-part ‘practice bundle’ achieved 30% incidence reduction across 15 hospitals
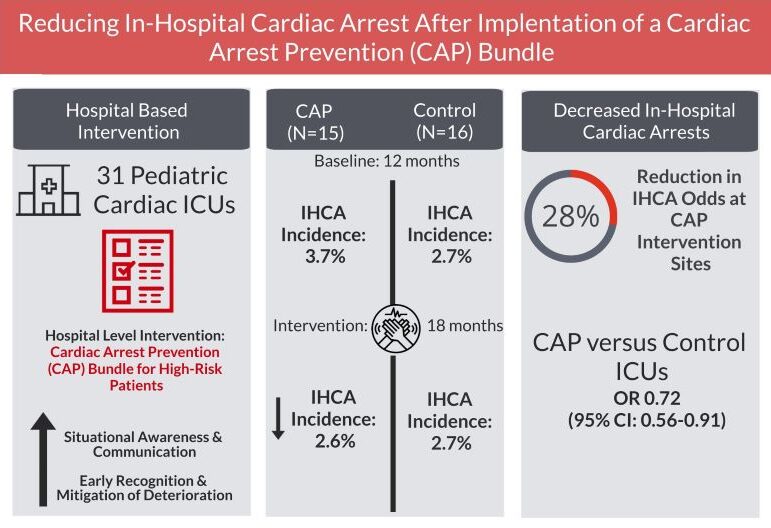
Despite years of investment to improve CPR and post-resuscitation care, many experts in the field have considered in-hospital cardiac arrest (IHCA) a largely unavoidable outcome for some children in cardiovascular intensive care units (CICUs). A recent study led by researchers at Cincinnati Children’s Hospital Medical Center and 14 other hospitals, challenges that notion.
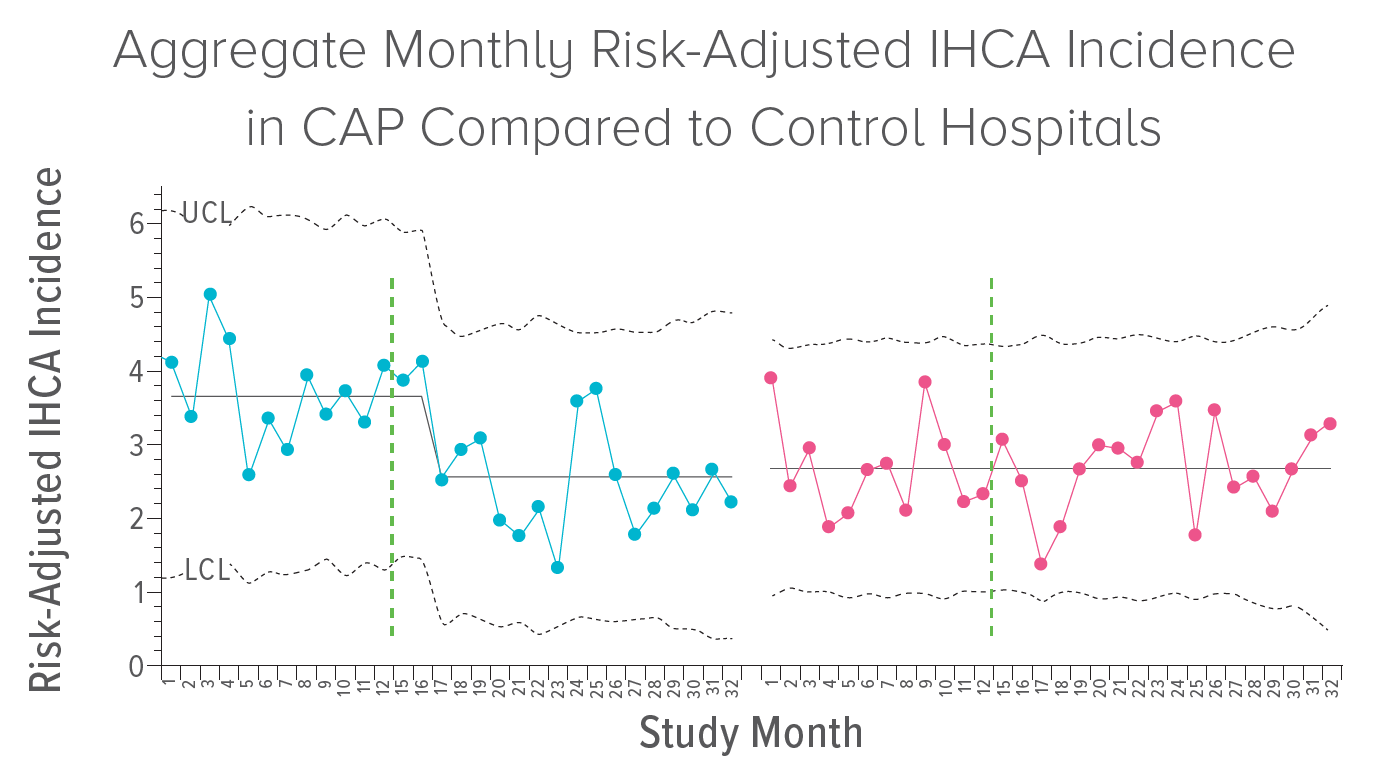
In a study published July 5, 2022, in JAMA Pediatrics, this group of investigators report that implementing a low-technology cardiac arrest prevention (CAP) practice bundle reduced IHCA incidence by an average of 30% across the participating centers. The results exceeded a targeted 25% reduction, and the practice changes used can be replicated in any institution, say project leaders Jeffrey Alten, MD, an attending physician at Cincinnati Children’s CICU, and Michael Gaies, MD, medical director of the Acute Care Cardiology Unit at Cincinnati Children’s.
The study reports the results of a quality improvement initiative that was conducted within a collaborative learning network of CICU teams across the Pediatric Cardiac Critical Consortium (PC4), which aims to improve the quality of care to patients with critical pediatric and congenital cardiovascular disease in North America and abroad. PC4 is part of Cardiac Networks United (CNU), a collaborative pediatric and congenital cardiovascular research and improvement network. Formed in 2017, CNU provides infrastructure for discovery and improvement work to participating networks which is scalable to accommodate a diverse group of collaborative partners and data sources.
“This study represents the culmination of years of effort by so many within PC4,” says Gaies, who was the founder and Executive Director of PC4 during the study. “We collaborated with hospitals across the country to collect data and understand variation in performance on IHCA prevention. Leaders from these institutions then came together to improve the quality of care across hospitals.”
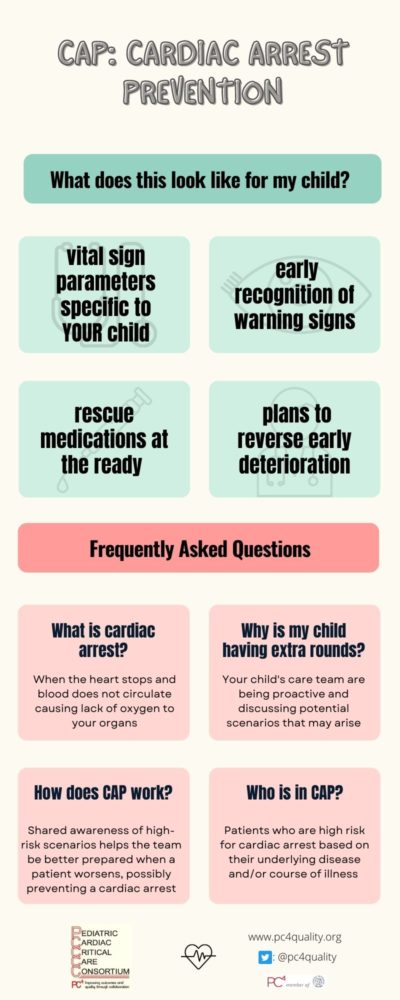
The CAP bundle was designed to promote situational awareness and communication to recognize and mitigate deterioration in high-risk patients. Each element of the bundle was specifically chosen to be minimal in cost and technology independent, allowing CICUs to adapt to their local system, QI resources, and clinical workflow. The bundles were comprised of five elements, including a mandatory twice-daily safety huddle.
Elements of the CAP Bundle
CAP Safety Huddle
This formal, multidisciplinary bedside discussion occurs separately from patient rounds and is designed to create situational awareness amongst the entire care team for high-risk patients. The huddle, which occurs twice each day, includes a bedside nurse, nurse leader, attending physician, first-responding provider, and respiratory therapist. Primary topics of discussion must include the most likely reason for an IHCA with a particular patient as well as mitigation and rescue plans. The goal is for the entire team to recognize early deterioration and agree on plans for reversal and/or rescue of a patient.
Vital Sign Discussion
This discussion can occur during the CAP Safety Huddle and seeks to establish parameters for patient-specific vital sign goal/targets, defining changes that may represent early deterioration. These parameters are posted in the patient’s room and programmed into the monitor and require bedside clinician evaluation and reassessment if there are changes to these parameters.
Discussion of Pre-sedation
This element also occurs during the CAP Safety Huddle and regards the use of pre-sedation for noxious stimuli since patients with tenuous conditions are more likely to suffer hemodynamic collapse related to agitation or pain. Compliance of this is based on the discussion, not ordering pre-sedation agent.
Emergency Medication
Since many IHCA episodes are preceded by acute hypotension, rapid administration of epinephrine may rescue a patient prior to cardiac arrest. The bundle calls for patient-specific doses to be pre-drawn and stored at the bedside.
Formal Code Review
This element dictates that a review of all cardiac arrests be reviewed within two weeks of the event – and ideally within 48 hours. Clinical staff involved in the event should be present during the review and key learnings and improvement opportunities should be disseminated to the rest of the medical and nursing staff.
Study Implementation and Analysis
Monthly webinars led by CAP project leaders featured education, data review, and collaborative learning to empower teams towards successful implementation. “This CAP project represents the first multicenter initiative aimed directly at IHCA prevention; and its success was made possible by the collaborative learning network formed by the 15 PC4 CAP hospitals,” says Alten. “Belief still persists that IHCA is an inevitability of critical illness, but as early adopters of the CAP bundle overcame obstacles and shared their improvement learnings on these webinars, this dogma was challenged, and confidence steadily increased among once reluctant participants that IHCA is indeed preventable. Proving feasibility of IHCA prevention represents the most essential message of this project, and hopefully will encourage spread of these IHCA prevention practices at other hospitals.”
The team ultimately analyzed data from 41,204 admissions, including 10,510 admissions at CAP hospitals, with 2664 of CAP admissions receiving the CAP bundle for an average of 4.4 days per patient. For all admissions at CAP hospitals, there was a 30% relative reduction in IHCA incidence rate during the intervention period, which translated to an average of 11 fewer IHCA events per month at CAP hospitals.
“Pediatric cardiac patients are at the highest risk of suffering in-hospital cardiac arrest with very high morbidity and mortality following the arrest event,” says Tia Raymond, MD, pediatric cardiologist at Medical City Children’s Hospital in Dallas. “High quality cardiopulmonary resuscitation during cardiac arrest combined with post-resuscitation care has been the focus, yet preventing a cardiac arrest all together in this high-risk population should be the priority.
“Our results from this multicenter collaborative among PC4 sites have demonstrated that identification of high-risk cardiac populations is possible, and that with implementation of a simple bedside cardiac arrest prevention bundle can result in significant reduction of cardiac arrest in this population. Our hospital has continued to identify and enroll patients in the CAP bundle and we have achieved to date a reduction in our cardiac arrest rate of 49% since implementation of the CAP bundle in May 2018 in our CICU.”
Next Steps
Researchers in the study say this represents an important paradigm shift in critical care to prioritize IHCA prevention and reduce adverse events. “The best CPR is no CPR,” says Alten. “And this project was able to prevent CPR in almost 200 high-risk children during CAP implementation at these 15 hospitals.”
Future studies are needed to determine which bundle elements are most necessary for cardiac arrest prevention and more work is needed to roll out the care bundle to more hospitals. Also, while the details of interventions would vary, the team leaders say the core elements of this bundle likely can be adapted to other critically ill populations, such as general pediatric and adult intensive care patients, and adult cardiovascular ICUs.
About the study
Participating centers were: Cincinnati Children’s Hospital Medical Center, Children’s National Hospital, Johns Hopkins Children’s Center, Medical City Children’s Hospital, Le Bonheur Children’s Hospital, Children’s Mercy Hospital, Dell Children’s Medical Center of Central Texas, Primary Children’s Hospital, Children’s Wisconsin, University of Alabama at Birmingham, Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center, Phoenix Children’s Hospital, Benioff Children’s Hospital, Seattle Children’s Hospital, University of Nebraska Medical Center Children’s Hospital and Medical Center, Arkansas Children’s Hospital, Nicklaus Children’s Hospital, Weill Cornell Medicine, Children’s Hospital Colorado, Medical University of South Carolina, Rady Children’s Hospital, and the University of Michigan.
Key funding sources included Children’s Heart Association of Cincinnati, Children’s Heart Foundation, and Castin’ ‘N Catchin’ Charity Organization via Children’s of Alabama.
View more discoveries from 50 research divisions and areas
Return to the 2023 Research Annual Report main features
| Original title: | Preventing Cardiac Arrest in the Pediatric Cardiac Intensive Care Unit Through Multicenter Collaboration |
| Published in: | JAMA Pediatrics |
| Publish date: | July 5, 2022 |
Research By