Cardiac Stem Cell Therapy Improves Scar Formation Rather Than Prompting Cardiomyocyte Regeneration
Post Date: March 22, 2021 | Publish Date: Nov. 27, 2019

“The implications of our study are very straightforward and present important new evidence about an unsettled debate in the field of cardiovascular medicine.”
— Jeffery Molkentin, PhD
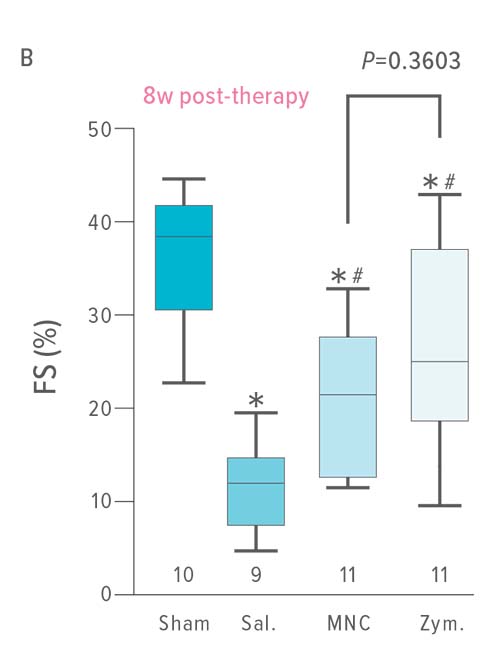
Stem cell therapy helps hearts partially recover from a heart attack by triggering an immune response that results in better scar formation and improved performance of surviving tissue—not by helping hearts grow new muscle.
This finding, led by Jeffery Molkentin, PhD, Director of Molecular Cardiovascular Biology at Cincinnati Children’s, helps clarify why a number of stem cell therapy trials have produced disappointing, but not entirely negative results.
The work by Molkentin and first author Ronald Vagnozzi, PhD, reveals an unexpected way that the heart responds to cardiac stem cell injections. Instead of the stem cells being integrated into the heart to grow cardiomyocytes as originally hoped, the injections trigger inflammation and an aggressive response from the body’s macrophage cells.
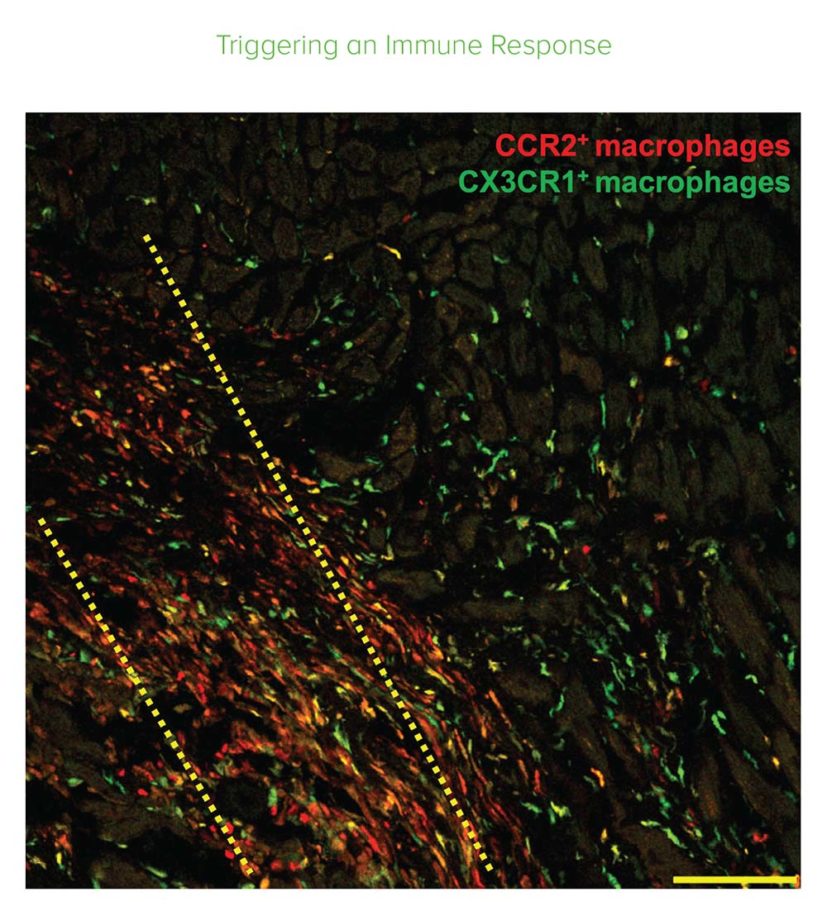
“The innate immune response acutely altered cellular activity around the injured area of the heart so that it healed with a more optimized scar and improved contractile properties,” Molkentin says. “The implications of our study are very straight forward and present important new evidence about an unsettled debate in the field of cardiovascular medicine.”
Molkentin, a Howard Hughes Medical Institute professor, made headlines in 2014 with a study in Nature showing that injecting c-kit positive heart stem cells into damaged hearts as a strategy to regenerate cardiomyocytes doesn’t work. This study reveals what happens instead.
AN UNEXPECTED DISCOVERY
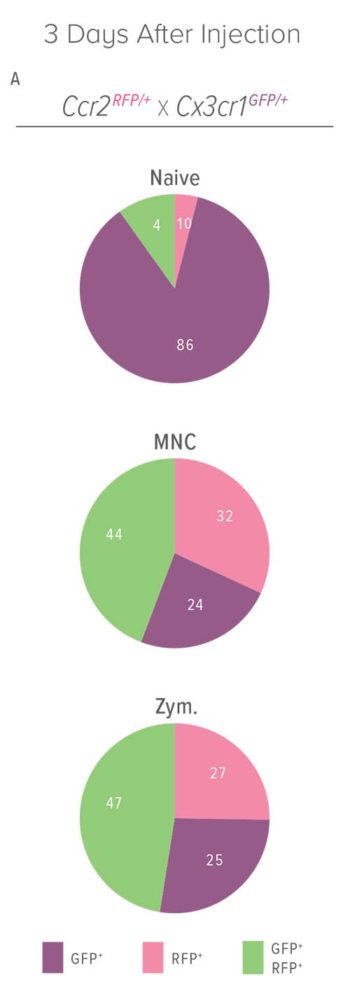
The study worked with mice using two types of heart stem cells—bone marrow mononuclear cells and cardiac progenitor cells. As the researchers tested their findings under different conditions, they discovered that live stem cells were not necessary for inducing the immune response they had seen. In fact, injecting dead cells produced the same outcome.
Further, they observed that zymosan, an inert chemical designed to induce an innate immune response, also provided a slightly greater and longer-lasting benefit to the heart than injecting stem cells or dead cell debris.
Be it stem cells or zymosan, the injections altered immune cell responses that significantly decreased the formation of extracellular matrix connective tissue in the injury areas, while also improving the mechanical properties of the scar itself.
The authors conclude: “Injected hearts produced a significantly greater change in passive force over increasing stretch, a profile that was more like uninjured hearts.”
The researchers also found that the response occurs only when the injections occur directly into the hearts, as opposed to infusing stem cells via the circulatory system.
“Most of the stem cell clinical trials were incorrectly designed because they infuse cells into the vasculature,” Molkentin explains. “Our results show that the injected material has to go directly into the heart tissue flanking the infarct region. This is where the healing is occurring and where the macrophages can work their magic.”
LOOKING TO THE FUTURE
Molkentin and colleagues plan to follow up these findings by looking for other ways to leverage the healing properties of the stem cells and compounds they tested.
For example, they plan to explore polarizing macrophages so that they exhibit only their healing-like properties.
Key collaborators included scientists in the Cincinnati Children’s Heart Institute, the University of Cincinnati, the Cardiovascular Research Center at Massachusetts General Hospital, and Harvard Medical School.
More Top 5 Achievements from the FY20 Research Annual Report:
-
Dose Escalation Sharply Improves Hydroxyurea Benefit for Children with Sickle Cell Anemia
-
World’s First Three-Organoid System Opens Doors for Medical Research and Diagnosis
-
Clinical Trial Success Caps Long Journey for HLH Treatment
-
Single Cell Approach Reveals Impact of Disease-Causing Gene Mutations
Read the full report
Request a PDF
| Original title: | An acute immune response underlies the benefit of cardiac stem cell therapy |
| Published in: | Nature |
| Publish date: | Nov. 27, 2019 |