Heart Assist Devices Making a Difference
Research By: David Morales, MD | Angela Lorts, MD | Ryan Moore, MD
Post Date: June 30, 2019 | Publish Date: June 2016

Oregon resident Susie Arroyo is pursuing her dream of becoming a teacher even as she battles Duchenne muscular dystrophy (DMD), thanks to a life-saving device that keeps her heart pumping.
Not long ago, the heart complications caused by her disease would have amounted to a death sentence for Susie. Instead, in March 2013, she became the second person in the U.S. with DMD to receive a ventricular assist device (VAD).
Before the surgery, “I couldn’t breathe. It was hard to even talk,” Susie says. With the device, “I have a lot of energy. My color is back…I feel like Susie again.”
In a world where donor organs for heart transplants remain in constant short supply, an evolving array of mechanical devices have begun to offer hope to more people with severe heart disease. Working together, doctors and scientists at Cincinnati Children’s are helping to expand the populations of patients that can be helped by these devices.
- Teens who have survived cancer, only to suffer heart damage later as a side effect of radiation and chemotherapy.
- Children born with DMD and other conditions that make them unlikely candidates for organ transplants.
- People stricken by acute infections in which an assist device can support them long enough for their own heart to recover.
The Heart Institute at Cincinnati Children’s has become one of the nation’s largest pediatric programs for mechanical-assist devices. In addition to offering families access to surgeons versed in working with multiple types of devices, the program trains other surgeons in how to install them.
Experts here have developed and shared innovative computer imaging tools to fit devices in as many younger, smaller children as possible. Surgeons and support teams here also do the complex work needed to be allowed to mix and match parts from different manufacturers so that devices can function in smaller chest cavities.
Meanwhile, experts in multiple fields within Cincinnati Children’s and colleagues in other medical centers are collaborating on research that could help patients live longer and better lives with mechanical devices.

“Even when children and teens get heart transplants, as many as 40 percent receive an assist device first. Otherwise, many would not make it to transplant,” says Angela Lorts, MD, Medical Director, Mechanical Circulatory Support at Cincinnati Children’s. “These devices can help some remain at home while they are on the waiting list, where they can focus on the nutrition and rehabilitation that will give them the strength they need for a successful transplant procedure.”
OTHER SUCCESSES INCREASE HEART ASSIST DEVICE DEMAND
As more children grow into adulthood after surviving cancer, as treatments for muscular dystrophies extend life, and as more children survive Fontan surgery and other rigorous procedures to repair complex congenital heart defects, many of these patients encounter heart complications decades later.
Mechanical devices will play important roles in extending life for these patients, which make innovations in device design and in long-term medical support all the more important. So far, surgeons at Cincinnati Children’s have implanted more than 50 cardiac-assist devices.
“We’re now starting to explore new patient populations who before had little to no hope,” says David Morales, MD, Chief of Cardiovascular Surgery at the Heart Institute. “We can support any child of any size with the best device for their particular heart failure.”

Customized Fitting Saves Lives
Cardiologist Ryan Moore, MD, did not start college dreaming of becoming a doctor. He started out as an art major intending to pursue a career in digital media.
But he found that he enjoyed science and that he wanted to apply his skills to help people in more direct ways. So, he switched to become a biology major and pursued medical school. Now, as a cardiologist, he uses his artistic skills in life-saving ways.
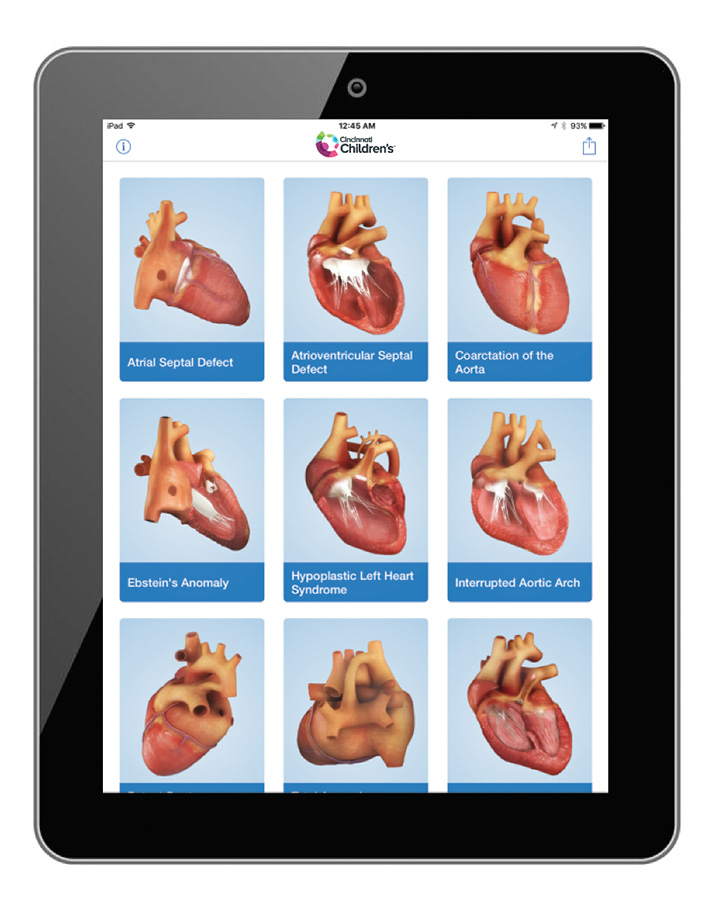
Moore was a leading member of a small team at Cincinnati Children’s that developed Heartpedia, a remarkable series of digital animations of major heart defects and the surgical procedures that can repair them. Moore also helped develop new software that allows experts to use CT and MRI scans to build rotating 3D images of an individual patient’s chest cavity.
Now, Moore and colleagues can use these tools to determine with precision whether a device will fit properly in smaller, younger patients. This approach allows significantly more children to receive devices safely compared to the existing standard based on body surface area (BSA).

Using BSA, few children under the age of 14 would be considered grown enough to receive a Syncardia total artificial heart or other large cardiac devices, Moore says. But with 3D fitting technology, children as young as 12—even some as young as 10—have been successfully fitted with devices.
“BSA is an extremely limited form of measurement for this purpose,” Moore says. “We have found that devices can be fitted in a number of children whose BSA measurements would preclude them. We also have found that the BSA measure sometimes can provide false positive results because it cannot account for chest cavities affected by scoliosis and pectus excavatum.”
In a recent study published in the June 2016 issue of the Journal of Heart and Lung Transplantation, Moore and colleagues used the 3D techniques to evaluate 15 patients who were rejected for Syncardia devices because their BSA exceeded 1.7 m2. The 3D imagery approach allowed eight of those patients to be fitted.
Looking ahead, Moore and colleagues are using these findings to begin rewriting the national eligibility criteria for heart devices.
A SOURCE OF HEART ASSIST DEVICE EDUCATION AND TRAINING
Cincinnati Children’s does not produce devices, but experts here play central roles in teaching both families and other medical centers about their use.
The Heartpedia mobile app provides clear visual depictions of heart conditions and procedures that many families find difficult to understand in other ways. The digital illustrations can be used in conjunction with 3D-printed heart models to explain how surgery will work.
“These visual tools have greatly enhanced our ability to communicate with families,” Moore says. “Not only do these tools help us during in-person meetings, families can take these videos and models home and explain things to other relatives, friends and caregivers.”
To measure the impact, Moore and colleagues are conducting follow-up studies to evaluate how much these visual tools improve understanding, in hopes that similar educational tools can be more widely shared.
Meanwhile, on the medical front, Cincinnati Children’s has taken visual training to another level by developing advanced computer simulation tools to train heart surgeons and care teams on how to work with ventricular-assist devices. So far, the training has been provided to more than 30 other medical centers.
“Virtual implantation has been critical to our success,” Morales says. “Until now, these devices have been designed almost exclusively with adults in mind. Now we are working with 11 other institutions to develop the pediatric protocols that will help standardize their use. This is an exciting and rapidly evolving field.”
Learn more about advanced heart surgery at Cincinnati Children’s
—By Tim Bonfield
(This article originally appeared in the Summer 2017 issue of Research Horizons.)
| Original title: | Virtual implantation of the 50cc SynCardia total artificial heart |
| Published in: | The Journal of Heart and Lung Transplantation |
| Publish date: | June 2016 |