Parental Stress, Depression Can Spike When Children with Brain Injury Develop Secondary ADHD
Research By: Megan Narad, PhD | Shari Wade, PhD
Post Date: August 1, 2022 | Publish Date: Aug. 1, 2022
Rehabilitation Medicine | Top Scientific Achievement

Traumatic brain injury (TBI) affects more than 500,000 children a year in the United States and often leads to cognitive, behavioral and social deficits. When TBI is combined with attention-deficit/hyperactivity disorder (ADHD), outcomes can be even more life-disrupting.
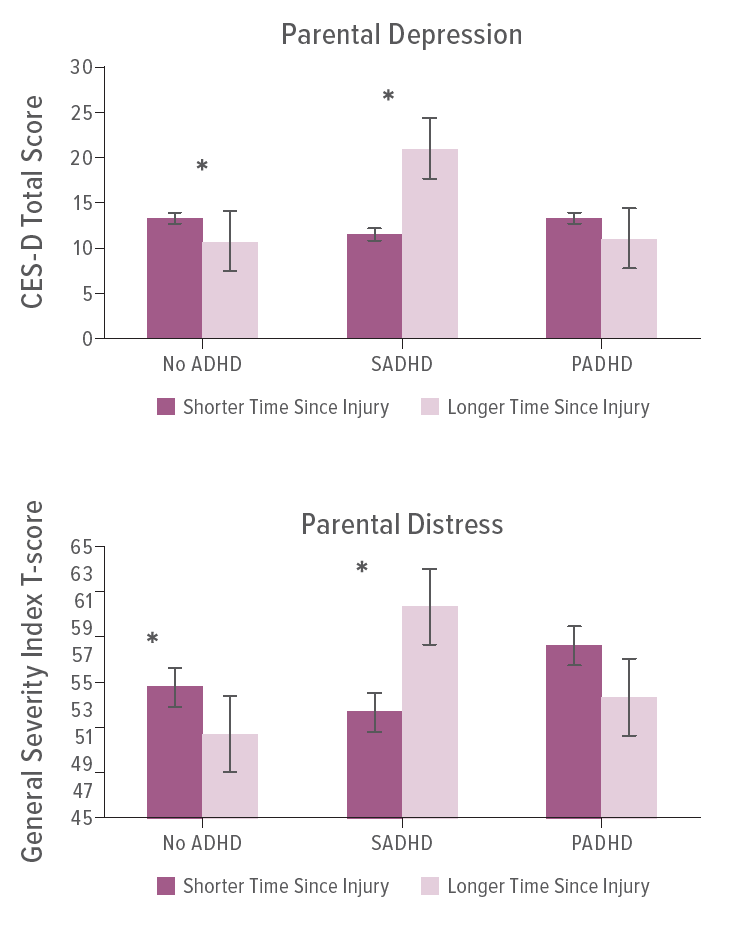
A study led by experts at Cincinnati Children’s found profound effects on executive function, social competence and functional impairment among children who had ADHD before their brain injury and among those developing ADHD as a secondary impact of brain injury. However, families of children who developed secondary ADHD, especially after severe TBI, also reported greater levels of parental distress and depression.
The findings reflect parent-reported data for 284 children, ages 11 to 18, who were hospitalized overnight at one of three medical centers for a moderate-severe TBI.
“The finding of greater parental depression and distress in the secondary ADHD group relative to both the pre-
injury ADHD and no ADHD groups was unexpected,” says corresponding author Megan Narad, PhD. “These findings underscore the importance of early identification and management of ADHD symptoms after TBI to mitigate long-term functional issues. The goal should be to intervene early and provide parents with strategies for managing difficult behaviors, and to prevent the cycle of new-onset behavior problems, increased parental distress, increased negative parenting strategies, and worsening of child behavior.”
More 2023 Research Highlights
Chosen by the Division of Rehabilitation Medicine
Wade SL, Walsh K, Slomine BS, et al. Widespread clinical implementation of the teen online problem-solving program: Progress, barriers, and lessons learned. Front Rehabil Sci. 2023;3:1089079. Published 2023 Feb 7. doi:10.3389/fresc.2022.1089079
Wade SL, Sidol C, Babcock L, et al. Findings from a Randomized Controlled Trial of SMART: An EHealth Intervention for Mild Traumatic Brain Injury. J Pediatr Psychol. 2023;48(3):241-253. doi:10.1093/jpepsy/jsac086
Smith-Paine J, Moscato EL, Narad ME, et al. More to the story than executive function: Effortful control soon after injury predicts long-term functional and social outcomes following pediatric traumatic brain injury in young children. J Int Neuropsychol Soc. 2023;29(4):325-335. doi:10.1017/S1355617722000315
Treble-Barna A, Wade SL, Pilipenko V, et al. Brain-derived neurotrophic factor Val66Met and neuropsychological functioning after early childhood traumatic brain injury. J Int Neuropsychol Soc. 2023;29(3):246-256. doi:10.1017/S1355617722000194
Torrens JN, Hetzer SM, Evanson NK. Brief Oxygen Exposure after Traumatic Brain Injury Hastens Recovery and Promotes Adaptive Chronic Endoplasmic Reticulum Stress Responses. Int J Mol Sci. 2023;24(12):9831. Published 2023 Jun 6. doi:10.3390/ijms24129831
View more discoveries from 50 research divisions and areas
Return to the 2023 Research Annual Report main features
| Original title: | The Impact of Preinjury and Secondary Attention-Deficit/Hyperactivity Disorder on Outcomes After Pediatric Traumatic Brain Injury |
| Published in: | Journal of Developmental & Behavioral Pediatrics |
| Publish date: | Aug. 1, 2022 |
Research By







