Vitamin D Supplementation Alleviates IL-13–Induced Esophageal Inflammation
Research By: Michael Brusilovsky, MMedSc, PhD | Marc Rothenberg, MD, PhD
Post Date: August 2, 2022 | Publish Date: Aug. 2, 2022

Vitamin D levels in the population have dramatically decreased, with 50% of the Western population being vitamin D insufficient (serum levels <30 ng/mL). Vitamin D deficiency has been linked with the risk and severity of numerous inflammatory diseases, including allergies and inflammatory bowel diseases.
Scientists at Cincinnati Children’s now report--in findings published Aug. 2, 2022, in Gut–that vitamin D supplementation may alleviate allergic inflammation in the esophagus, whereas vitamin D deficiency may lead to a higher risk of developing allergic states, such as the severe food allergy eosinophilic esophagitis (EoE).
The team performed a series of experiments involving mouse models and human samples to detail the involvement of vitamin D in counteracting allergic inflammation at the molecular level.
The study is one of the latest in a growing body of evidence illustrating how human health depends in many ways upon sufficient vitamin D levels.
“As vitamin D is considered an essential factor required for healthy immune responses and has many effects on various tissues, including the skin. Its deficiency may have profound effects on human health and disease,” says corresponding author Marc Rothenberg, MD, PhD, Director, Division of Allergy and Immunology and the Center for Eosinophilic Diseases at Cincinnati Children’s.
The Rothenberg CURED laboratory focuses on deciphering the pathogenesis of allergic diseases and development of precision-based therapies derived from understanding mechanisms of disease.
In this study, investigators examined the impact of vitamin D on allergic inflammation in the esophagus.
A specific role for vitamin D
“One of the remarkable findings in the study was that vitamin D supplementation did not have a dramatic effect on vitamin D deficient conditions in a healthy state; however, in the vitamin D deficient and allergic state, vitamin D supplementation reversed IL-13-induced responses thought to be germane to EoE , reducing epithelial hyperproliferation and intercellular spaces and improving barrier function,” says the study’s lead author, Michael Brusilovsky, MMedSc, PhD.
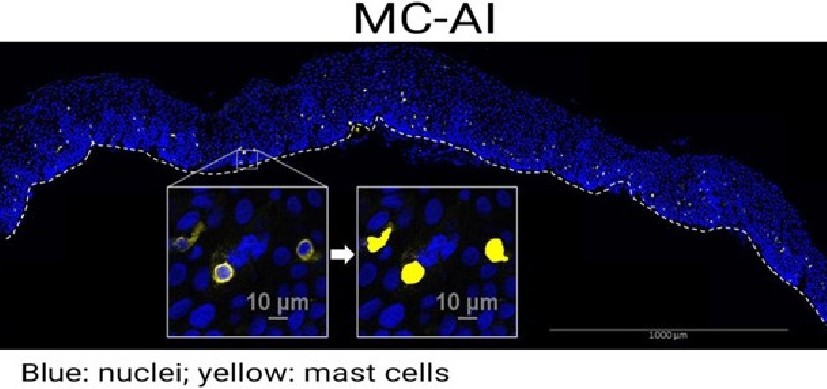
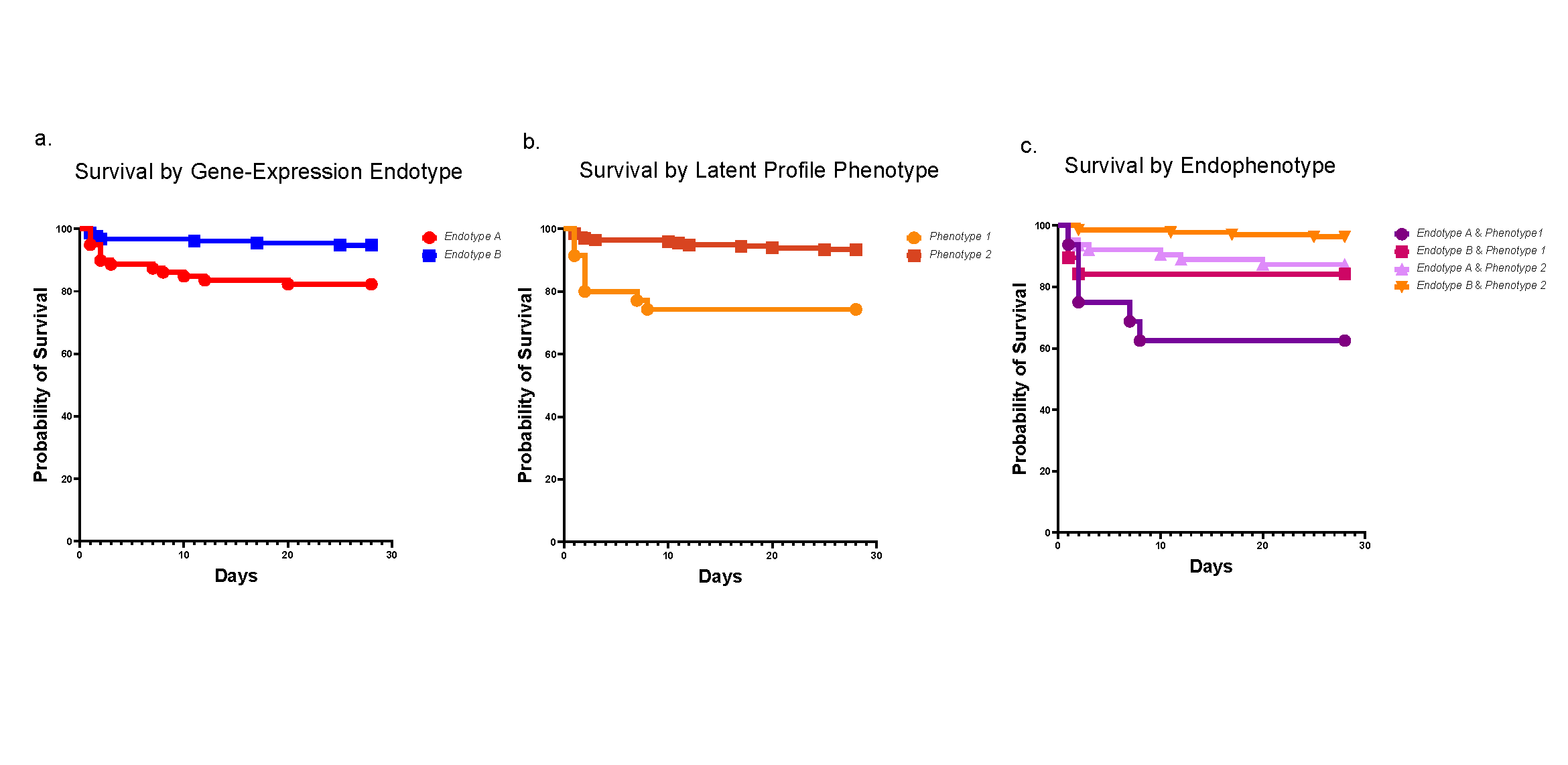
The study involved assessing the genomic distribution and function of the cellular vitamin D receptor (VDR) and STAT6 using histology, molecular imaging, motif discovery and metagenomic analysis. Metagenomic analysis showed that vitamin D supplementation reversed dysregulation of up to 70% of the transcriptome and epigenetic modifications (H3K27Ac) induced by IL-13 in vitamin D–deficient cells, and VDR and STAT6 co-localized within the regulatory regions of the affected genes, suggesting that the VDR and STAT6 interactome governs epithelial tissue responses to IL-13 signaling.
The team further demonstrated in preclinical model of IL-13-mediated esophageal allergic inflammation and in human EoE that vitamin D levels inversely associated with severity of esophageal eosinophilia and epithelial histopathology.
These findings in the esophagus adds to a large body of research to help alleviate allergic diseases.
Looking ahead, the research team plans to translate the findings—which overall identify vitamin D as a natural IL-13 antagonist with capacity to regulate the esophageal epithelial barrier functions, providing a novel therapeutic entry point for type 2 immunity–related diseases—for preventive and restorative medicine and therapies. These findings have translational significance as IL-13 blockers are now in clinical usage, including for EoE, and vitamin D is available for oral and topical delivery.
About the study
In addition to Brusilovsky and Rothenberg, Cincinnati Children’s co-authors included Mark Rochman, PhD, Tetsuo Shoda, MD, PhD, Michael Kotliar, MS, Julie Caldwell, PhD, Lydia Mack, MS, John Besse, MS, Xiaoting Chen, PhD, Matthew Weirauch, PhD, and Artem Barski, PhD.
This work was supported in part by the National Institutes of Health (R01AI045898, R01AI130033, R01AI123176, and R01AI113125); the Campaign Urging Research for Eosinophilic Disease (CURED); and the Sunshine Charitable Foundation and its supporters, Denise and David Bunning.
Read More About EoE Research at the Rothenberg CURED Lab
| Original title: | Vitamin D Receptor and STAT6 Interactome Governs Esophageal Epithelial Barrier Responses to IL-13 Signaling |
| Published in: | Gut |
| Publish date: | Aug. 2, 2022 |
Research By