A New Kind of Clot Blocker
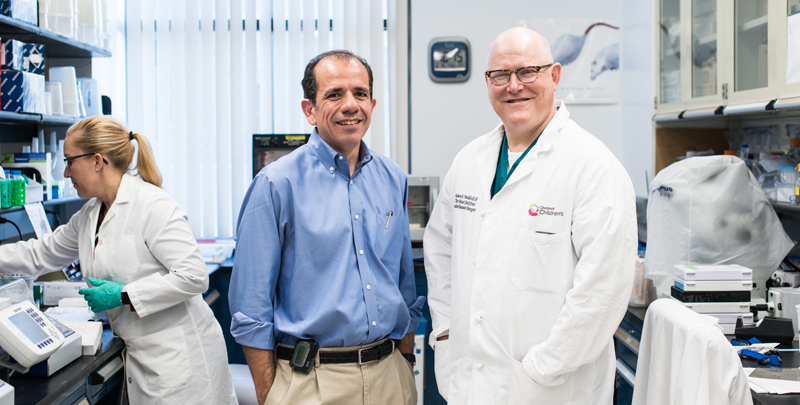
Research By: Joseph Palumbo, MD | James Tweddell, MD
Post Date: June 30, 2019 | Publish Date: October 2018
“If this approach succeeds, a person receiving a cardiac device would be protected from contact-mediated clotting but could still undergo future surgeries, or heal from accidental trauma, with greatly reduced risk of bleeding.”
—Joesph Palumbo, MD
Every surgeon who has connected a patient to a heart-lung bypass machine, placed an infant on an ECMO pump, or installed one of the growing number of mechanical heart support devices on the market has faced this battle:
How to prevent deadly blood clots from forming without creating an also-deadly risk of bleeding?
Decades ago, doctors and scientists learned that blood rapidly begins to clot when it contacts metal parts, glass and plastic tubing, and other non-biological materials. For many years, doctors have reduced the risk of clots by employing large doses of heparin, warfarin or other anti-coagulants.
The well-known problem has been that the balancing act can easily fail, leading either to clot-triggered strokes or severe internal bleeding events. The longer a person’s blood is in contact with a device, the harder it becomes to avoid a complication.
“When the first Berlin Hearts were introduced, there was a very high clotting rate, as high as 20 to 25 percent,” says James Tweddell, MD, Executive Co-Director of the Heart Institute at Cincinnati Children’s. “If it were possible to prevent clots effectively without incurring a bleeding risk that would be an enormous improvement.”
Now, just such a solution may be on the horizon.

Tweddell, an internationally-prominent cardiac surgeon, is collaborating with Joseph Palumbo, MD, an expert on blood and blood diseases at Cincinnati Children’s, on early-stage research that zeroes in on blocking “contact activation” of the clotting cascade. Their work indicates that inhibiting the function of coagulation factor XII (F12) can prevent device-related blood clotting while not affecting the body’s ability to heal wounds.
A key factor for the future of cardiac devices
With only a few thousand donated organs available per year, receiving a full heart transplant is not a realistic option for the hundreds of thousands of people in the United States coping with heart failure. These include children born with severe heart defects, young adults battling diseases such as Duchenne muscular dystrophy, and legions of seniors with hearts weakened by previous heart at-tacks, coronary disease, and age.
For most who reach advanced heart failure, the hope of extended life depends heavily on mass-producing practical cardiac support and replacement devices. When that day arrives, device recipients might be able to live on for years, even decades—but they will not live well if they must depend on existing anticoagulation therapy.
“Even the newer anticoagulants that have been developed in the past five to 10 years come with significant bleeding risks,” Palumbo says.
In the last decade, however, researchers have been learning more about how F12 works, and how it relates to other clotting factors. That work has led Palumbo, Tweddell and colleagues to evaluate a compound made by California-based Ionis Pharmaceuticals.
Targeting factor XII to block pathological clot formation
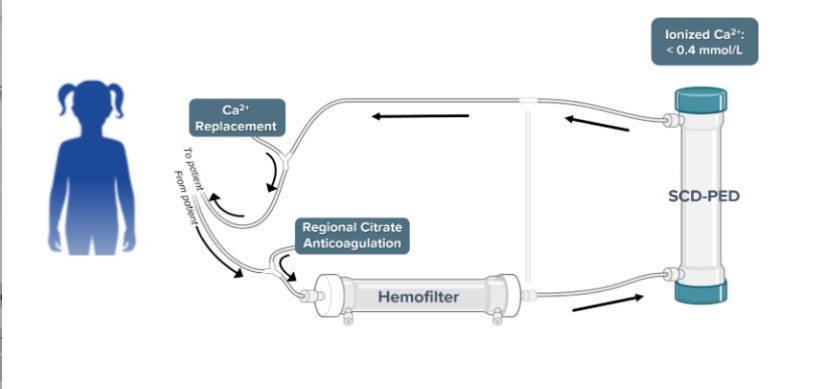
Clot formation, Palumbo says, is the final step of a cascade of activity involving multiple blood proteins.
Older anticoagulant drugs, such as heparin and warfarin, act like massive dams toward the bottom of this cascade. (See Figures A, B and C.) They interfere with the production and/or function of thrombin, the central protein in the clotting cascade needed for making fibrin, the material that actually forms clots.
By blocking the activity of proteins later in the clotting process, current anticoagulants significantly impair patients’ ability to form any kind of clot, desired or not. The new approach would place the dam on a side stream—before it joins the larger cascade, Palumbo says.
While F12 is crucial to how the blood reacts to foreign surfaces, it plays no role in stopping the bleeding associated with wounds. Thus, blocking only F12 would allow the rest of the cascade to flow unimpeded, and carry no surgical bleeding risk.
“If this approach succeeds, a person receiving a cardiac device would be protected from contact-mediated clotting but could still undergo future surgeries, or heal from accidental trauma, with greatly reduced risk of bleeding,” Palumbo says.
To test their hypothesis, these researchers are using an exciting potential treatment that relies on a “gapmer,” a type of antisense oligonucleotide (ASO) that can be used to silence the function of a specific gene. Gapmers are highly specific, and can be used for extended periods. The gapmer produced by Ionis specifically targets the gene controlling F12.
“By suppressing the contact activation pathway, this treatment could allow use of bypass machines, ECMO, ventricular-assist devices, and so on, with much less than standard anticoagulation,” Tweddell says.
Early-stage testing underway
A lab team including Farhan Zafar, MD, research associates Scott Baker, Leah Rosenfeldt, and Malinda Frederick, clinical veterinarian Brenda Wynn, and surgical veterinary technician Savannah Walters have begun testing the F12-blocking compound in preclinical models.
So far, the work is showing promising results that appear to serve as a basic proof of concept. However, much more testing is needed before clinical trials can begin, Palumbo says.
Next steps
More testing is needed to verify the early results, Palumbo says. Further rounds of study would likely involve longer time frames and more types of cardiac assist devices.
The highly-specific gapmer approach could be ideal for long-term management of ventricular assist devices. Patients (or caregivers) would even be able to administer treatments at home. However, the weeks-long build-up period needed before surgery could be a limiting factor for the gapmer approach when it comes to bypass surgery. A faster-acting F12 inhibitor would be beneficial for patients facing more urgent situations.
“Even if this approach cannot fully replace the need for heparin or warfarin, any large reduction in the dosages of those drugs would have a potentially dramatic impact on bleeding risks,” Palumbo says.
| Original title: | Gene Silencing - A Strategy for Anticoagulation during Mechanical Circulatory Support |
| Published in: | Congenital Heart Surgeons' Society, 46th Annual Meeting |
| Publish date: | October 2018 |