A Deeper Commitment to Health Justice and Eliminating Health Inequities
Research By: Andrew Beck, MD, MPH | Robert S. Kahn, MD, MPH | Carley Riley, MD, MPP, MHS | Ndidi Unaka, MD, MEd
Post Date: January 24, 2024 | Publish Date:

New Michael Fisher Child Health Equity Center to Build Partnerships, Expand Research to Address Structural Challenges that Perpetuate Health Inequities
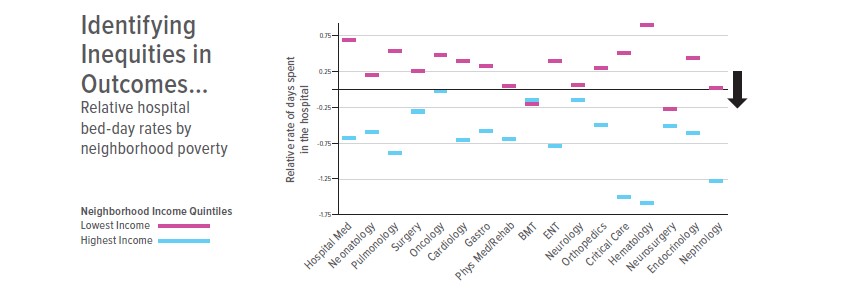
Robert Kahn, MD, often shares a chart that looks like an old computer programming punch card but actually paints a sobering portrait of the health inequities that children face while living within a few miles of the nation’s No. 1 pediatric health system.
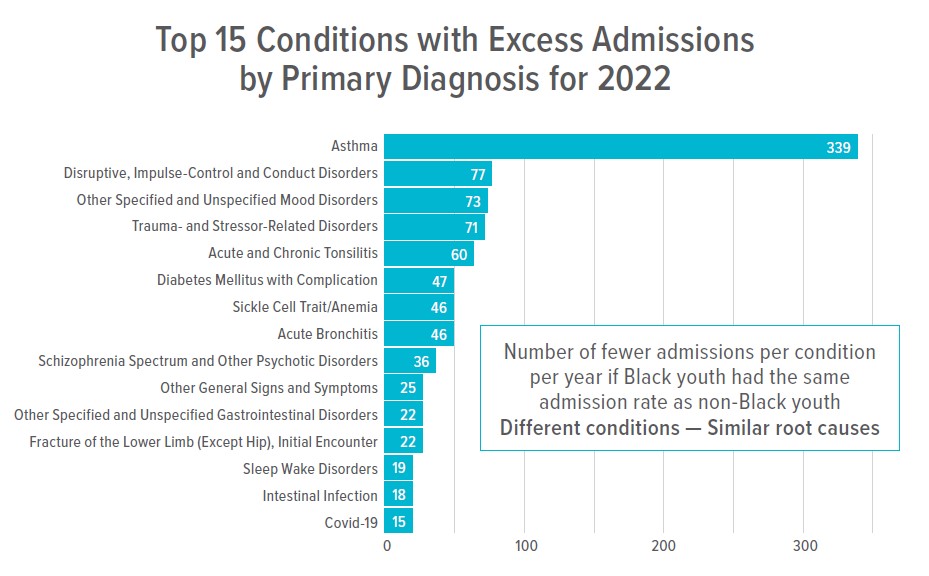
The chart shows obvious differences in the relative number of days children spend in the hospital for a variety of conditions from asthma emergencies to psychiatric stays to extreme preterm birth.
“You don’t need to get into the fine print to see that for every subspecialty, lower income kids are spending more time in the hospital than higher income kids,” says Kahn, the inaugural director of Cincinnati Children’s new Michael Fisher Child Health Equity Center.
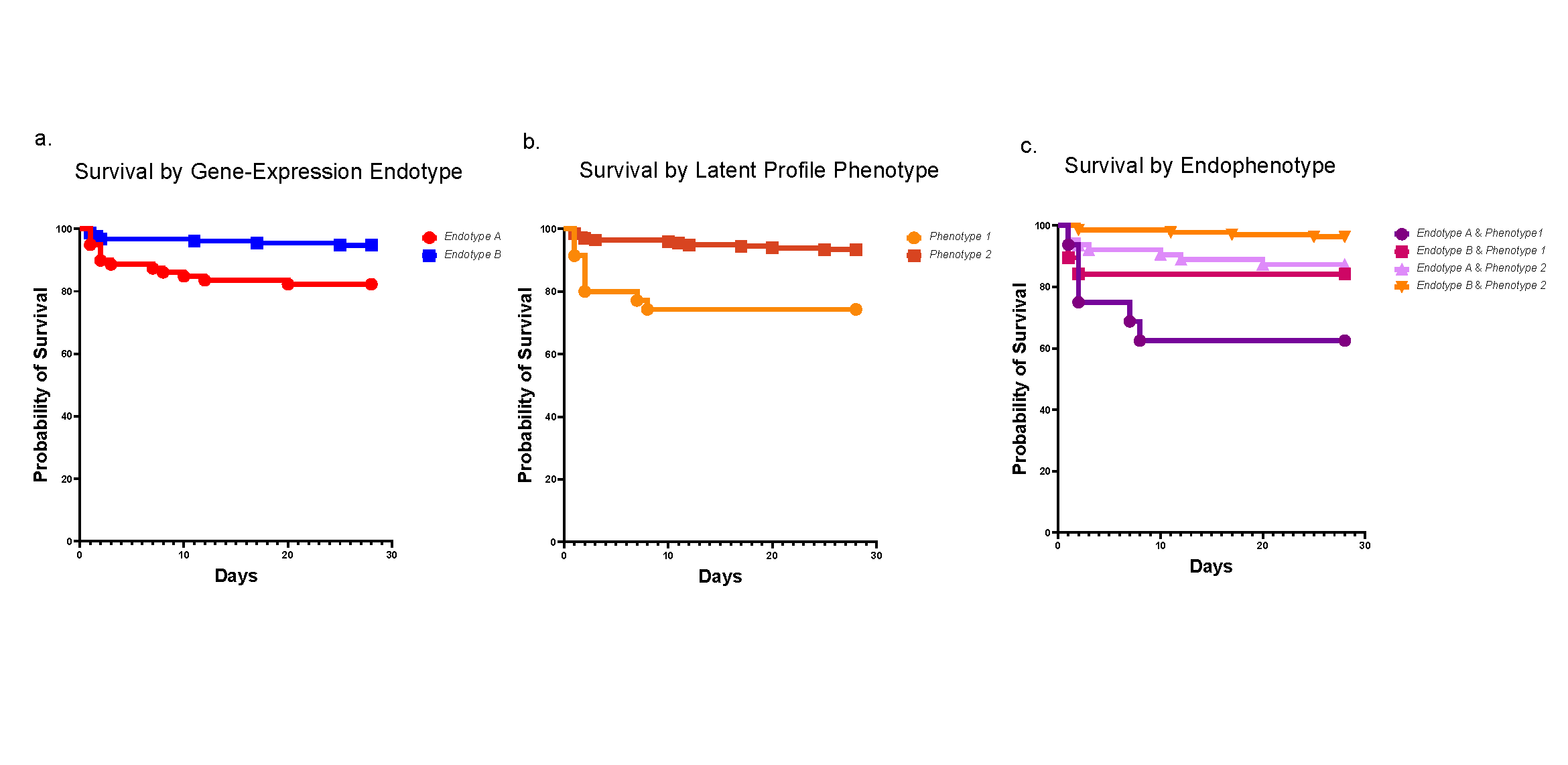
Flash to another chart, and glaring racial inequities are documented in terms of how many fewer days of high-cost hospital stays would be required if Black children had the same rate of hospital admissions as non-Black children. It’s not just for admissions; similar inequities are seen for birth outcomes, early child development and kindergarten readiness.
“Clearly, even though we are the No. 1 children’s hospital in the country not every child is benefiting,” Kahn says. “Even as we consider a wide array of outcomes, we find that the root causes for most of the inequities are the same. So how do we organize as an institution to partner as part of a larger community system to get the work done to reduce these inequity gaps?”
Mission to Help All Children Reach Full Potential
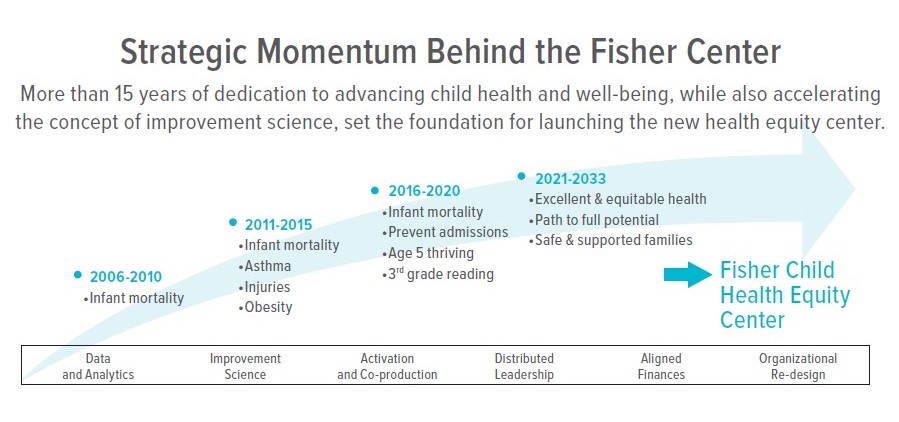
The Fisher Center was announced in late 2021; Kahn was named director in September 2022. He and a diverse group of internal and external stakeholders worked to define the Center’s new vision, mission and priority initiatives.
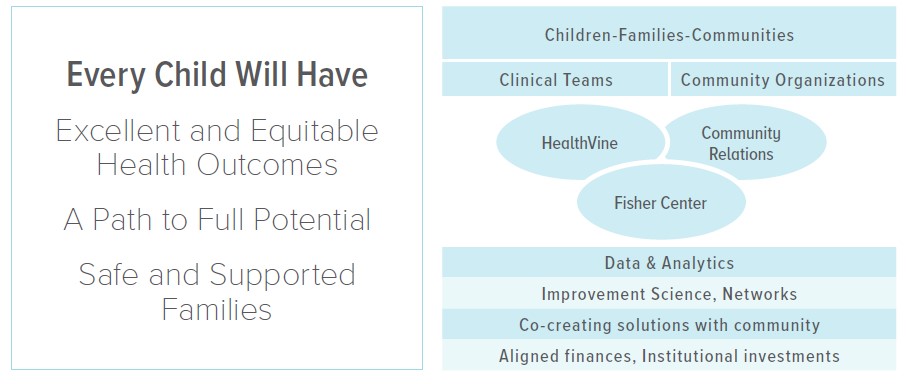
The vision for the Fisher Equity Center builds directly on the vision for Cincinnati Children’s in seeking to ensure that all children and families reach their full potential. The Center also carries forward the Pursuing our Potential Together 2033 Community strategic plan themes: ensuring that all children have excellent and equitable health outcomes and a pathway to achieve their full potential, and that all families are safe and supported.
The Fisher Center embraces several guiding strategies:
- Amplify child, youth and family leadership, agency, and voice
- Support a healthcare system that pursues equitable outcomes as part of an integrated, family-centered community-wide network
- Partner to create community conditions that promote equitable child and family well-being outcomes
- Advance learning, research and system change in ways that promote equity and challenge injustice.
In previous Community Health strategic plans, hospital leaders successfully worked with community stakeholders to advance focus on population health priorities. Infant mortality rates in Hamilton County have been significantly reduced. Asthma hospitalization rates across the county decreased. The days children from Avondale and Price Hill spent hospitalized decreased. The Cincinnati Child Health-Law Partnership, a collaboration with the Legal Aid Society of Greater Cincinnati, has led to a 40% reduction in hospitalizations, in part by prompting legal actions against owners of unhealthy apartment buildings.
The Fisher Center aims to scale these efforts and catalyze new ones.
Internal partnerships will also be critical. Cincinnati Children’s recently established the Office of Population Health. This office oversees a Medicaid accountable care organization called HealthVine to support coordinated, value-based health care. The Anderson Center brings world class expertise in quality improvement. The institution has launched strategic plans for Diversity, Equity and Inclusion and Community Relations. And the Office of Academic Affairs and Career Development has spurred increases in the percentages of new faculty hires from underrepresented populations.
The Fisher Center represents the next big leap forward at Cincinnati Children’s to bring these many important threads of progress into a full tapestry that can foster a bolder impact on community health and health equity.
Catalyzing our Equity Journey for Greater Impact
The center is named after Michael Fisher, who retired in 2021 from his role as president and CEO. Throughout his decade-long tenure, Fisher championed the concept that all of Greater Cincinnati’s kids should rank among the healthiest in the nation.
That goal has yet to be achieved but remains a driving force behind our equity journey.
Some of the center’s work involves bolstering connections to grow an institutional culture around equity. This means sharing best practices for equitable care, addressing common root causes of inequities in partnership with families and communities, and accelerating research and innovation to determine what interventions work well and can be scaled up to share beyond Cincinnati. But the key element of the entire effort is partnership with the community.
“Achieving equitable health outcomes is not something Cincinnati Children’s can do alone. Our role is to bring medical and scientific expertise to the table, but the goals, the plans, the actions and leadership depend upon establishing and re-establishing trust at many levels,” Kahn says. “This is about accepting collective responsibility for results that matter to children and families. This is about working at every step with community partners to co-create the conditions in the health system and the community that can foster equitable child outcomes.”
A Deep Research Dive
As fiscal 2024 continues, the Fisher Center’s leaders and collaborators are working on plans to reduce racial and socioeconomic inequities in hospital admission rates and newborn and infant outcomes. In concert, the center seeks to pursue equitable pathways to full potential by improving academic and developmental outcomes for all children, with a focus on closing equity gaps.
To do so, the center is expanding a system for community learning, including co-developed shared objectives, expanded parent and institutional capabilities, connected data, and built intentional partnerships. The focus is initially on some of Cincinnati’s most structurally disadvantaged neighborhoods, with the eventual goal to scale and spread.
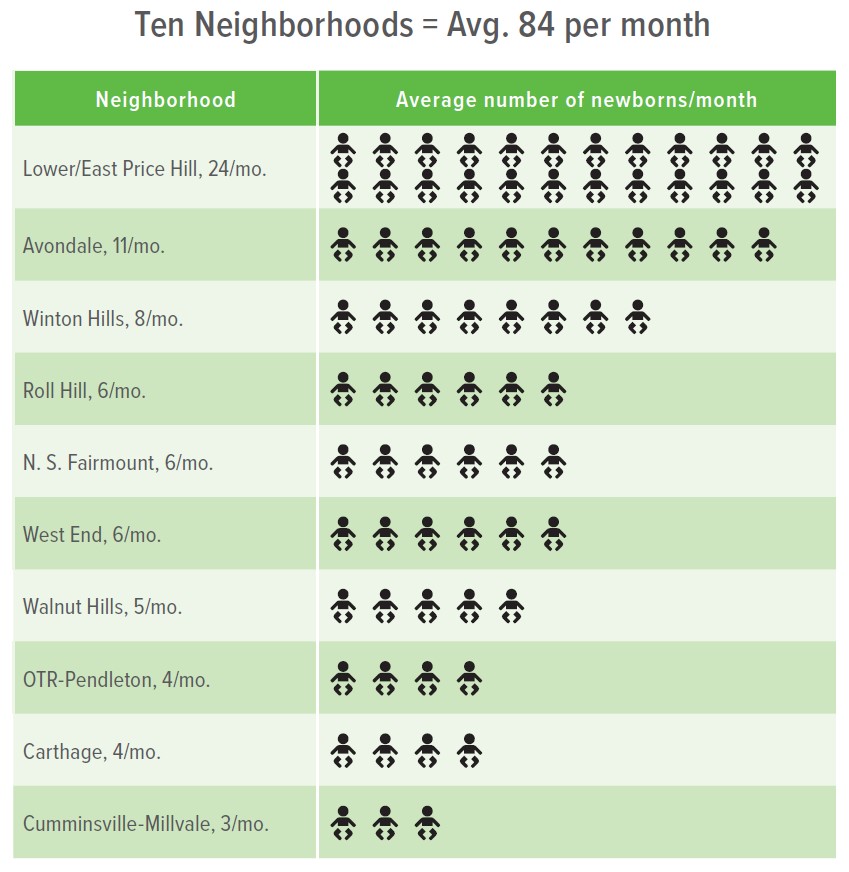
A focus on certain neighborhoods helps align partners around common denominators – the 103 asthma admissions from these neighborhoods that occur each year; the 84 babies born in these neighborhoods each month. How would an equitable system improve outcomes across a range of physical and mental health conditions? What needs to change to help each of every baby get on a trajectory that allows them to achieve their fullest developmental potential? What can we learn in a single neighborhood, or set of neighborhoods, that could be scaled to our city, our region, and beyond?
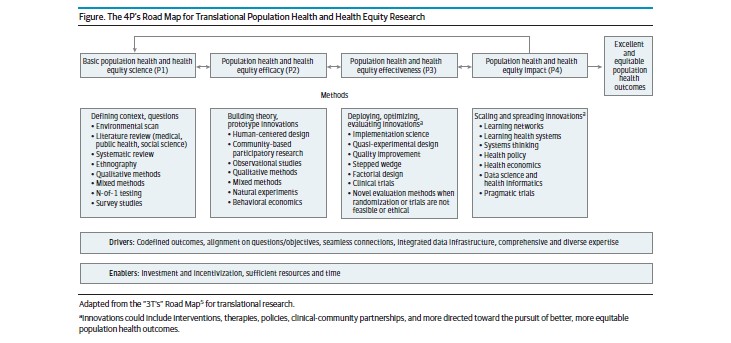
“To achieve health equity across the life course, we know that we have to ensure that our children are born, grow and live in environments that produce an equitable trajectory,” says Carley Riley, MD, MPP, MHS, our faculty lead for Community Systems Science. “Our theory is that by creating a cross-sector learning system led by families and community members we’ll be able to design, implement and evaluate meaningful, sustainable health equity interventions and systems transformation.”
So far, the Fisher Center team has worked with families and community leaders to identify and define key aspects of a more equitable health system. This means that success will be measured not just by reductions in hospital admission days, but also by determining how close the system gets to a “north star” model that is antiracist, easily accessible, empathic, empowering of families, integrated, proactive, safe, and trustworthy.
“Health care is just one node in the larger community system needed to ensure that all children and their families can thrive. It is in this community space that the social, economic and political influences on child health play out. Cincinnati Children’s doesn’t need to lead that work but it can bring its research and innovation expertise,” Kahn says.
Indeed, the Fisher Center believes that learning networks will be central to achieving success. They are well suited to solving complex problems and have been used in the context of improving patient safety and chronic conditions. The learning network model used by the Fisher Center seeks to have patients, families and communities directly shape prioritized outcomes, help articulate the research questions and co-develop and test the needed interventions. Community partners, such as the Cincinnati Health Department, are already playing critical roles in the network.
Cincinnati Children’s will be increasing internal funding for priority studies and recruiting new faculty to accelerate the work. A significant aspect of the mission includes training and mentoring faculty and community partners to bolster community co-production of population health and health equity research.
Excellent and Equitable Health
One key initiative of the Fisher Center, with support and collaboration from the Office of Population Health, is the Health Equity Network. Led by Andrew Beck, MD, MPH, and Ndidi Unaka, MD, MEd, it brings together experts from numerous specialties to organize and share core services that clinical practices will need to accelerate equity. This work includes connecting clinical leaders, uncovering root causes of inequities, supporting increased response to social needs, and building a library of innovations for use across different care settings. Health Equity Network teams are supported by quality improvement, data, and community engagement specialists to catalyze learning and action.
The Health Equity Network includes 10 teams from across Cincinnati Children’s actively pursuing equity-oriented improvement aims. Example interventions include the spread of Legal Aid to subspecialty clinics.
“Over the years, we’ve experienced a great deal of success with our medical-legal partnership in primary care. But we know that many children and families receiving care from subspecialists also stand to benefit. The Health Equity Network provides a vehicle for testing such spread,” says Beck, who directs Population Health/Health Equity Research and Innovation in a shared role between the Office of Population Health and the Fisher Center.
The new HealthVine organization provides a fiscal and administrative structure for accelerating equitable outcomes. This network of pediatric care providers provides care management, quality improvement and utilization management for about 120,000 children and young adults covered by Medicaid in eight Ohio counties.
“HealthVine can contribute to the reduction of racial and socioeconomic equity gaps that exist across a number of diagnoses, including asthma, mental and behavioral health conditions, and Type 1 diabetes,” says Unaka, who serves as Medical Director for Quality Improvement and Analytics for Population Health and Faculty Lead for Health Care Equity for the Fisher Center. “It can do so by deploying care managers and community health workers to support families, and by testing interventions that would otherwise not be supported in fee-for-service models. The link between the Fisher Center and Population Health allows us to do so much more together than we ever could do apart.”
What will success look like?
Expect to see progress measured in many ways, be it real-time dashboards of key equity indicators, expanded training courses that reach beyond Cincinnati Children’s walls, growth in grant funding, scientific publications, and more.
Ultimately, the hope is that a day will come when a child’s race or ZIP code is no longer a predictor of their health outcomes. However, it won’t be scientists and clinicians deciding whether success has occurred. That, Kahn says, will be an impact assessment reserved for families and communities.
View more discoveries from 50 research divisions and areas
Return to the 2023 Research Annual Report main features
Research By

I help lead Cincinnati Children’s community health initiative which seeks to equitably optimize child health outcomes.