Study: Improved Chemotherapy and Surgery Eliminating Need for Radiation for Low-Grade Gliomas
Research By: Peter de Blank, MD
Post Date: March 4, 2024 | Publish Date: March 1, 2024
Successful outcomes from evolving surgical and chemotherapy treatments for pediatric low-grade glioma (pLGG) have greatly reduced the need to perform radiation therapy for this type of brain tumor, according to a recent study published in Nature Cancer.
The study, led by corresponding author Peter de Blank, MD, MSCE, co-medical director at Cincinnati Children’s The Cure Starts Now Brain Tumor Center, explored how changing forms of therapy has affected long-term outcomes in adult survivors of childhood gliomas. Pediatric low-grade glioma (pLGG) is the most common brain tumor in children, accounting for approximately one-third of brain tumors diagnosed annually in the United States.
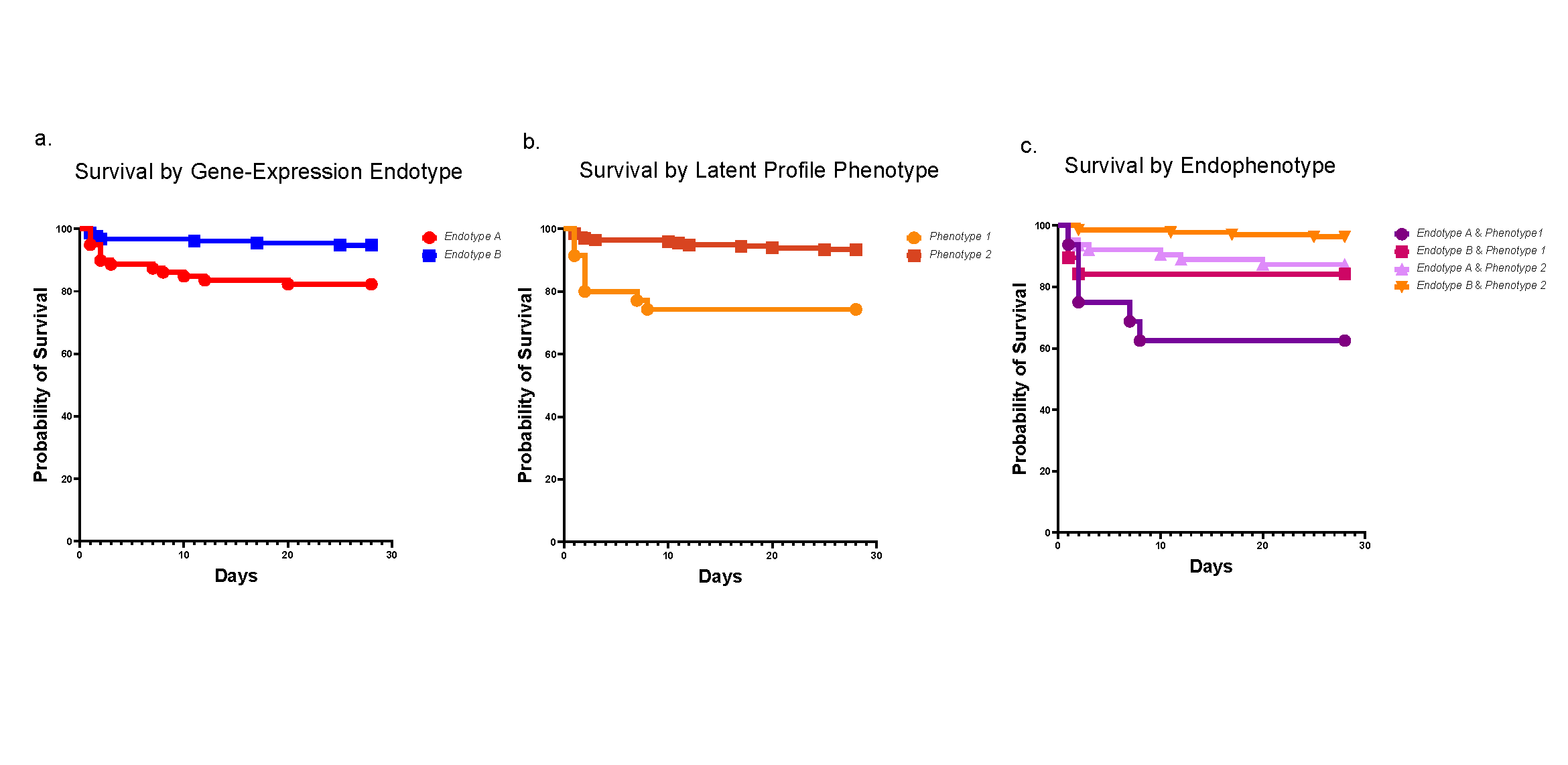
The study followed 2,501 adult survivors of pediatric glioma diagnosed in the 1970s, 1980s and 1990s. The patients were followed for an average of 24 years (range 5-48 years). From the 70s to the 90s, the proportion of survivors exposed to cranial radiation went down (62.6% to 26%), while the proportion exposed to surgery alone or surgery with chemotherapy increased.
Over the three decades, the risk of late mortality, chronic health conditions and subsequent neoplasms among survivors of pediatric glioma decreased with time. When researchers included treatment in the model, however, the effect of time decreased. This shows that some of the improvements in outcomes for pediatric glioma over time are a result of changes in how these patients are treated.
“Radiation works very well and stops gliomas from growing most of the time,” de Blank says. “The problem is that it has multiple side effects associated with radiation that don’t always come out immediately.”
Moving away from radiation and towards chemotherapy and surgery is responsible for much of the improvements in late outcomes over time. Other reasons why outcomes have improved over time likely include better screening and survivorship care, the advent of MRI and improvements in radiation and surgical techniques. More recent advances, like proton radiation therapy that reduces the amount of healthy brain exposed to radiation, are too new to be included in this study.
“We also looked at whether delays in radiation improved late outcomes,” de Blank says. “Over the same three decades, the proportion of survivors who received delayed radiation (a year or more from diagnosis) increased from 3.2% to 30.1%, suggesting that treating physicians were trying to delay radiation when possible.”
However, delayed radiation was not associated with better outcomes (late mortality, chronic health conditions, subsequent neoplasm) or fewer reports of impaired learning or concentration. It may be that a longer delay is needed to see important effects, or that the most important thing is to avoid radiation altogether whenever possible.
Overall, the study shows that reserving radiation for pediatric low-grade glioma with no other options has improved late outcomes for survivors. Current therapeutic studies, such as ACNS1833 (led by Dr. de Blank) will help determine if newer targeted chemotherapy will further improve outcomes and quality of life compared to traditional chemotherapy.
| Original title: | Temporal changes in treatment and late mortality and morbidity in adult survivors of childhood glioma: a report from the Childhood Cancer Survivor Study |
| Published in: | Nature Cancer |
| Publish date: | March 1, 2024 |
Research By

My clinical and research interests include children with central nervous system tumors, neurofibromatosis type 1 (NF1), and NF1-related tumors. My research focuses on the investigation of tissue microstructure in pediatric brain tumors through non-invasive imaging techniques such as MR relaxometry and diffusion tensor imaging.