Reducing Cardiac Arrests in the PICU by Improving Situation Awareness
Research By: Maya Dewan, MD, MPH
Post Date: November 2, 2021 | Publish Date: Aug. 20, 2021
Written by Maya Dewan, MD, MPH
It is said that “patients don’t suddenly deteriorate—healthcare professionals suddenly notice.”
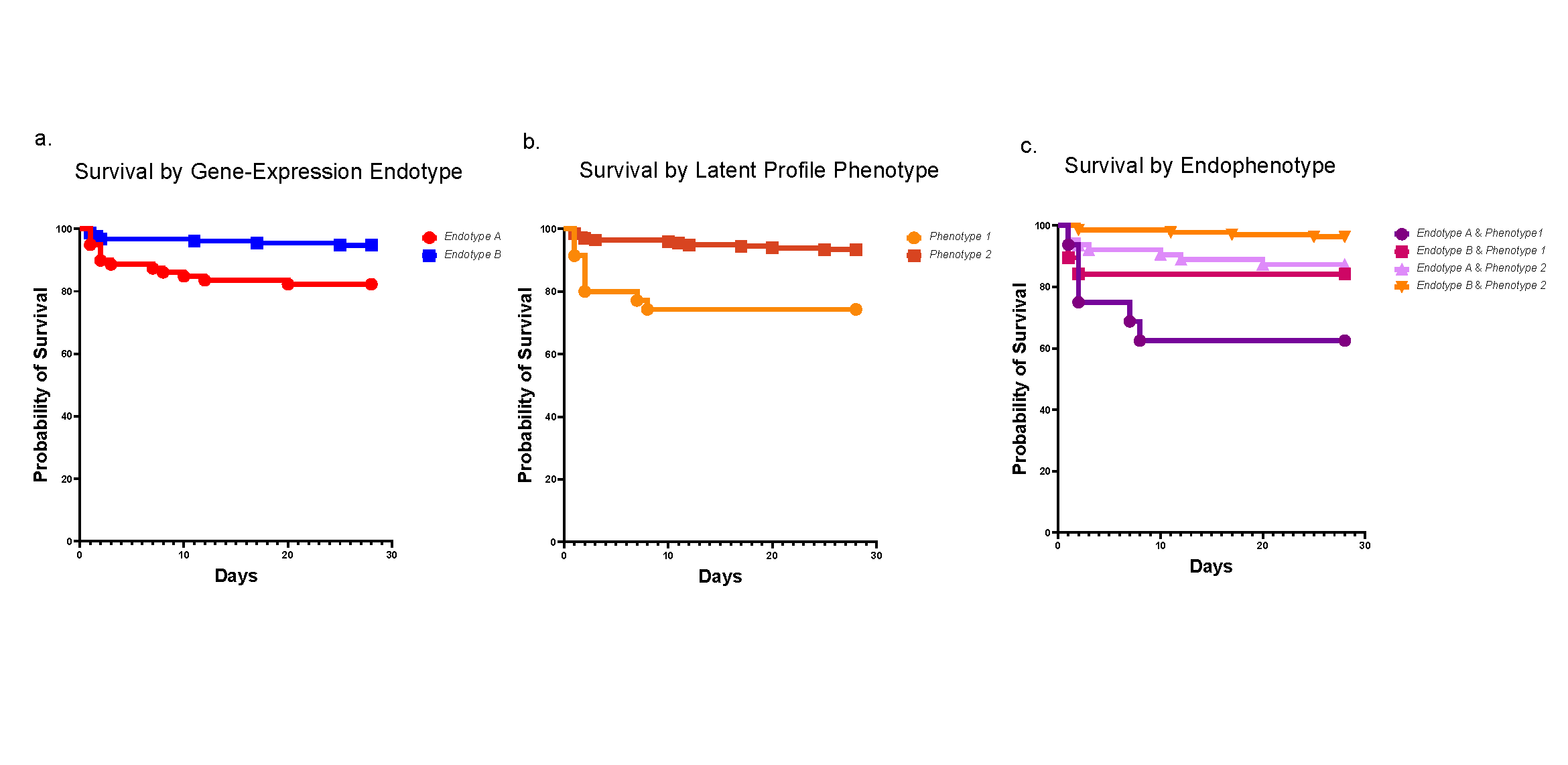
In a study published Aug. 20, 2021, in the journal Pediatric Critical Care Medicine, my colleagues and I demonstrated that through a shared understanding of patient risk and trajectory, we can prevent children from experiencing cardiac arrest in the pediatric intensive care unit (PICU). In the last year, this work led to 16 fewer children experiencing cardiac arrest at Cincinnati Children’s.
Previous work led by Patrick Brady, MD, MSc, research director of the Division of Hospital Medicine, focused on improving the situation awareness of our care teams and adapting this to the high-acuity and high-pressure world of ICU medicine. Based on this research, we were confident that improving situation awareness would improve care—however, we did not expect such a significant decrease in cardiac arrests, nor did we expect to see the large impact on mortality.
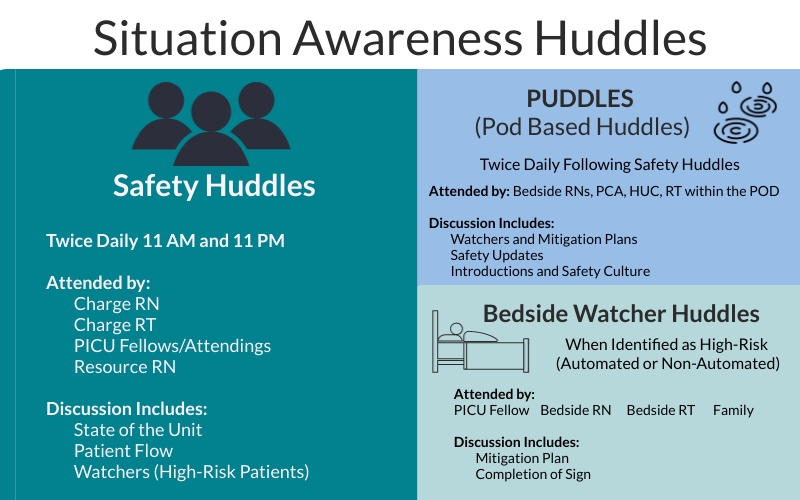
Our work began with a paper checklist to predict patients in the PICU at risk for cardiac arrest. From there, we automated the tool within the electronic health record (EHR) to improve the ease of its use for the entire care team. This study demonstrates that the use of such a tool combined with improved structured team communication can improve patient outcomes and save lives. Cardiac arrests are preventable—even for the sickest patients.
These outcomes push us to work even harder to further reduce these episodes and to expand this work to other care areas and hospitals. To be successful, this requires partnership between nurses, physicians, respiratory therapists, and unit leadership to identify high-risk patients and keep them safe. It also requires investment from the hospital to support the design and building of both automated tools and bedside signage.
Much of this work has already spread to acute care areas and other ICUs. In the next year, we plan to improve our standardization and automation. With a committed team and a culture of change, this system can be rolled out anywhere, even without the automated tool. The only requirement is a structured way to identify patients and a clear communication plan on how to mitigate risk and prepare staff.
As we move into the new Critical Care Building, we have worked to strengthen this system with improved visual displays. The color of the door sign will change for high-risk or “watcher” patients to provide a visual clue. New bedside mitigation plans with improved detail and clarity will be used to plan ahead and catch deteriorating patients before a cardiac arrest. Through our situation awareness work, the system of teamwork and communication will be further strengthened in this new building.
| Original title: | Assessment of a Situation Awareness Quality Improvement Intervention to Reduce Cardiac Arrests in the PICU |
| Published in: | Pediatric Critical Care Medicine |
| Publish date: | Aug. 20, 2021 |
Research By