Population Health & Equity: A Quest to Improve Outcomes for All Children
Post Date: January 24, 2024 | Publish Date:

How great can an academic medical center be if the innovations flowing from its laboratories fall short at improving health at community-wide, society-wide levels? The impact of medical advances cannot be measured solely by remission rates, survival years and symptom relief. Increasingly, the value of medical advancement must be examined through the lenses of affordability and equitable access to cutting edge care. Many experts here are committed to applying scientific rigor to efforts to improve the system, to deepening community engagement, advocating for change, and going well beyond the bedside to improve outcomes for children.
Be it addressing inequities in hospital care, remaining ever-vigilant about disease outbreaks, or applying research expertise in new ways to achieve population scale impact, science at Cincinnati Children’s extends well beyond our walls.

How Families Can Help Expose Blind Spots
Robyn Kinebrew, Tawanna Williams, Christian Lawson, and LaToshia Rouse didn’t need PhDs or MDs behind their names to earn their place as co-authors on a study published in February 2023 in The Journal of Hospital Medicine.
Instead, their courage to speak up about their lived experiences as Black people seeking hospital care for their children was more than enough to claim such recognition.
“My husband and I were always cognizant of what we wore when going to the hospital,” Kinebrew says. “He would change out of a t‐shirt and shorts into business causal so he wouldn’t be thought of as ‘a thug.’ When I was there alone, there was often an assumption that I was a single mom with no insurance.”
While the Kinebrews were seeking care for twins born with sickle cell disease, the Williams family had a child coping with congenital heart disease, Lawson was personally fighting Crohn’s disease, and Rouse had one child with autism and a set of triplets growing up with the complications that often come with preterm birth.
“As a Family Advisor in the NICU, I would coach Black families about talking with the care team. Black men tend to talk with their hands. I explained to them that that is seen as a threat,” Rouse says.
The fear of having hospital staff calling in Child Protective Services if a parent gets too emotional runs top-of-mind for Black families in ways that White families rarely expect to experience even though they may be just as loudly upset and worried about their children.

The study detailing how Black families often carry unseen traumas into their hospital visits was part of the Roadmap Project, launched by the American Board of Pediatrics (ABP) and led by Carole Lannon, MD, MPH, of the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s. The project is part of the ABP’s strategic initiative to improve pediatric mental health, with Roadmap focused on the emotional health in children and youth with chronic conditions and among their families.
“This paper highlights the voices of lived experience and shares actionable strategies that clinicians, divisions, and health systems can make to address racism and ensure equitable care and support for Black families during hospitalization,” Lannon says.
Research to address systemic inequities in health care delivery, to engage with community members to co-create research objectives, to participate in learning networks of patients, clinicians and scientists working together, have been hallmarks of the Anderson Center mission since it was launched in 2010.
Now community-facing aspects of this work are accelerating with the formation of the Michael Fisher Child Health Equity Center, directed by Robert Kahn, MD.
Read more about the Roadmap Project research
Protecting the Public Despite COVID Fatigue
While politicians, the media, and many members of the public are more than ready to put the COVID-19 pandemic in their rear-view mirrors, health professionals cannot afford to take their eyes off a constantly mutating virus looking for any new opportunity to spread to more hosts.
In fiscal 2023, ended June 30, Cincinnati Children’s experts in the Division of Infectious Diseases, the Gamble Vaccine Research Center, and other centers and divisions here have authored or co-authored 26 scientific publications related to COVID and the ongoing effort to keep up with its alphabet soup of variants and subvariants. This work includes:


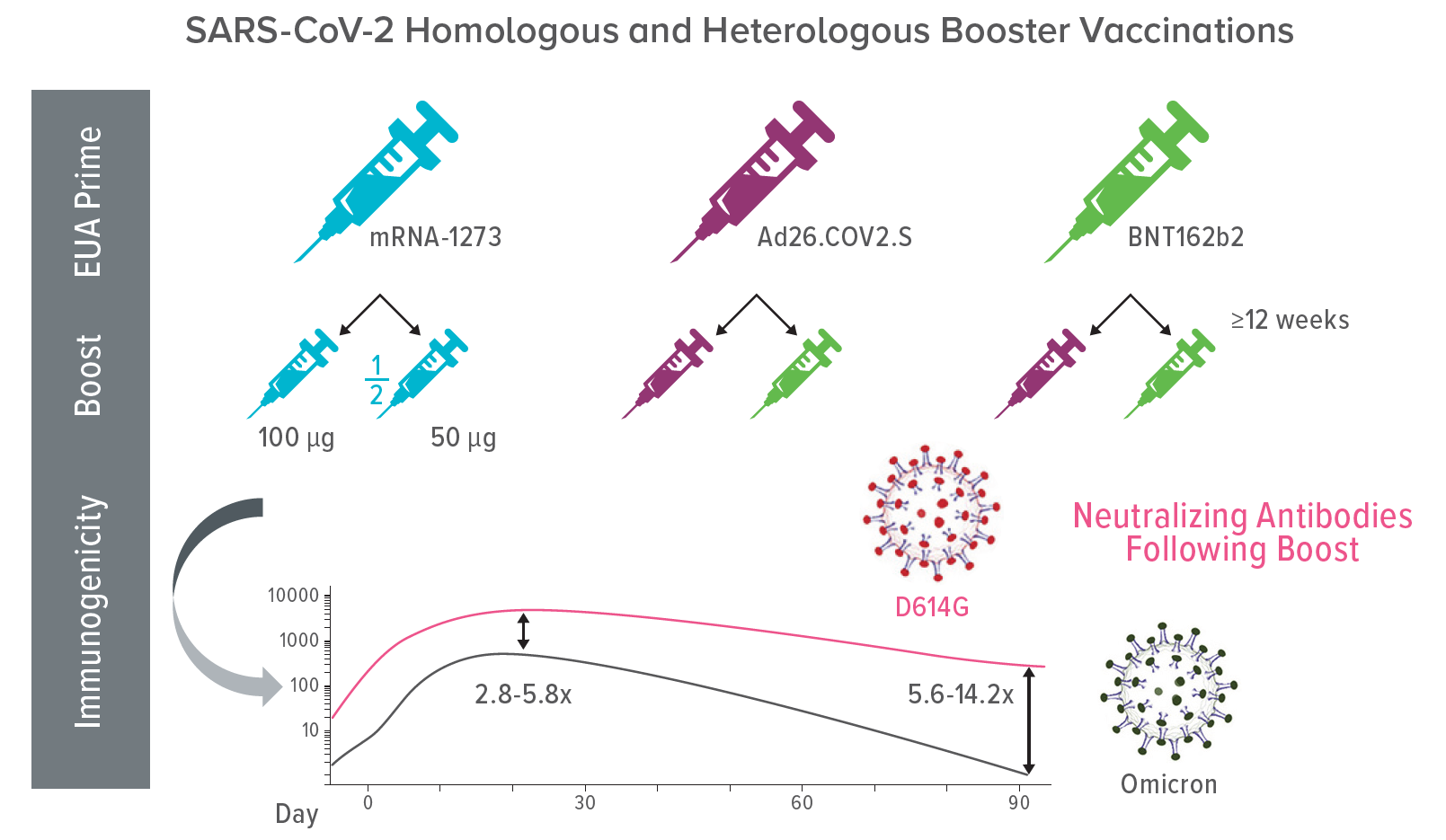
Rebecca Brady, MD, and Robert Frenck, MD, were among co-authors of a sobering manuscript published July 19, 2022, in Cell Reports Medicine that reported vaccine booster doses generating high levels of neutralizing antibodies against the Omicron variant, but a substantial decrease in those antibody levels within three months.
The findings, from an ongoing Mix and Match clinical trial, helped prepare the medical world and the public for the likelihood that COVID vaccination may become more like the annually adjusted influenza vaccine than the one-time vaccines that have offered long-term protection against other infectious diseases.

Mary Allen Staat, MD, MPH, was a Cincinnati Children’s representative in a large group of pediatric-focused experts called the “Overcoming Covid-19 Investigators.” In July 2022, this group published findings in The New England Journal of Medicine showing that fewer newborns needed hospital intensive care from a COVID infection when pregnant moms got vaccinations after 20 weeks gestation vs. earlier in pregnancy. But even that protection slipped as the virus shifted from the Delta to the Omicron variants.
More recently, Staat was a leading co-author for an NIAID-supported study that found sharply different immune responses in children vs. adults. Details were published in print Oct. 12, 2023, in the journal Cell.
In February 2023, Grant Paulsen, MD, served on the C4591007 Clinical Trial Group that reported in The New England Journal of Medicine confirming that the BNT162b2 vaccine was safe and effective for children under 5.




Then in April 2023, Staat and Elizabeth Schlaudecker, MD, MPH, served on an MIS-C review group that published findings in April 2023 in Pediatrics showing minimal adverse risk to teens who received the BNT-162b2 vaccine.
Melinda Butsch Kovacic, MPH, PhD, collaborated with several researchers at Cincinnati Children’s and the University of Cincinnati on a study addressing vaccine hesitancy that was published in July 2022 in the International Journal of Environmental Research and Public Health.
Meanwhile, Stephen Becker, PhD, addressed vaccine hesitancy in children with ADHD as a co-author of a study published in August 2022 in the Journal of Psychiatric Research.
How Serious is the Risk of Preterm Birth from Exposure to Phthalates?
Phthalates are pretty much everywhere. This class of chemicals that help make plastic products more durable can be found in a wide range of food containers, cosmetic products and more. Several of these endocrine-disrupting compounds have been banned or restricted in some nations and several U.S. states, but many other phthalates are not well-studied, nor well-regulated.

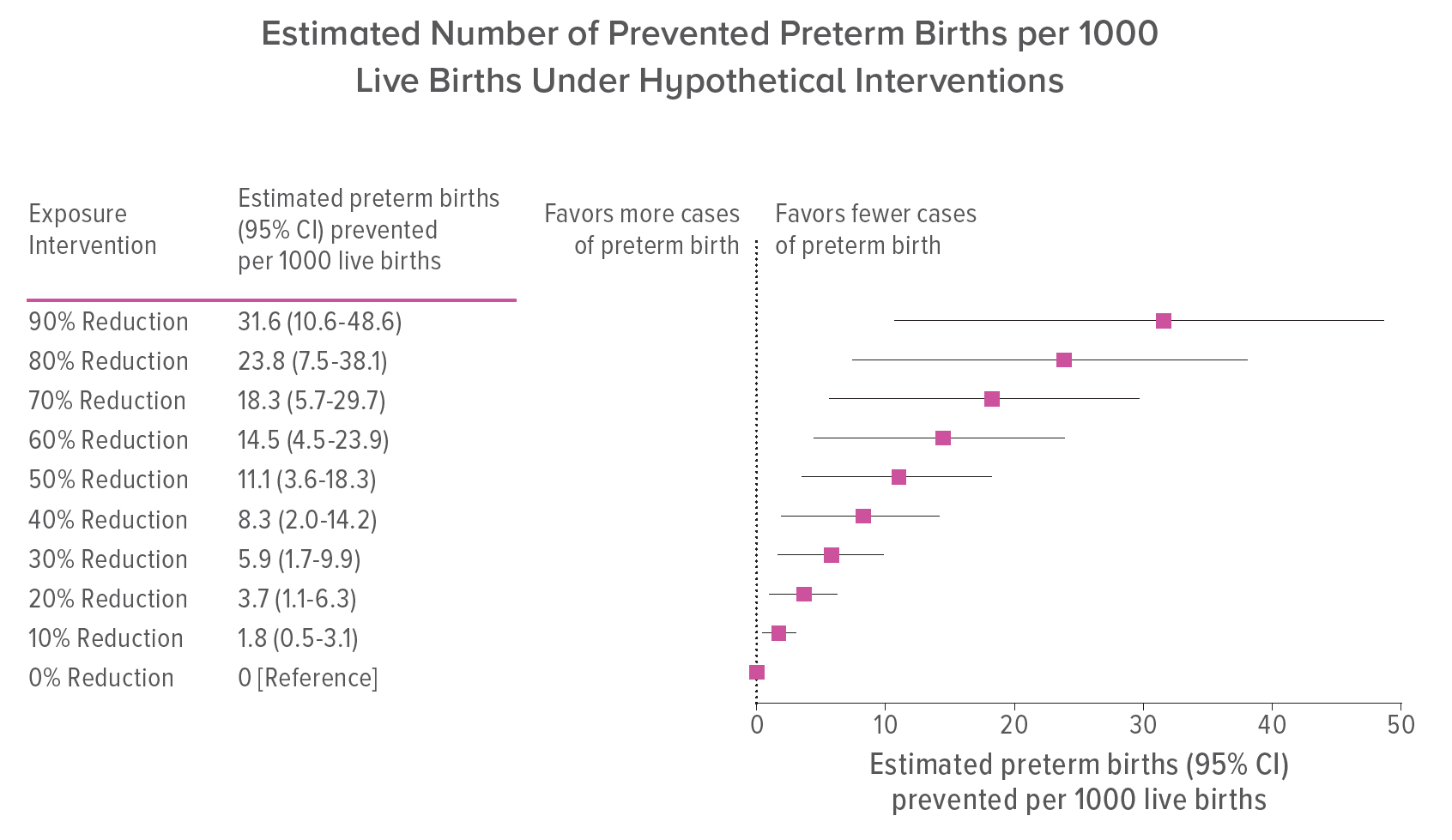
Developmental psychologist and epidemiologist Kim Yolton, PhD, has been studying the pediatric effects of these chemicals for years. In September 2022, she co-authored a study in JAMA Pediatrics that pooled the results of 16 cohorts of pregnant women (data spanning 1983 to 2018) to take a deeper look at how pregnancy may be affected by these exposures. The results were disturbing.
First, the study found that 96% of the study participants were exposed to detectible levels of phthalates, according to urinary biomarkers. But exposure levels varied, and risk of preterm birth were clearly associated with higher dose exposures.
Overall, the 6000+ women in the study experienced 90 preterm births per 1000 live births. Had it been possible to intervene at the time, the researchers say that two preterm births per 1000 could have been avoided with a 10% reduction in exposure. Six preterm births per 1000 could have been avoided with a 30% reduction in exposure. Meanwhile 11 preterm births per 1000 could have been avoided by cutting exposure levels by 50%.
In the US, various studies have shown that phthalate exposure varies widely by sociodemographic factors, including whether a person lives at a disadvantaged socioeconomic status or is of a particular marginalized race or ethnicity. Helping reduce exposures likely depends on a mix of behavior changes and regulatory actions, the paper states.
“Results from this large US study population suggest that phthalate exposure during pregnancy may be a preventable risk factor for preterm delivery,” Yolton and colleagues wrote.