Pediatric Trainees Use ‘Roadmap Project’ Tools to Address Emotional Health
Research By: Lori Herbst, MD | Sue Poynter, MD | Carole Lannon, MD, MPH
Post Date: September 5, 2024 | Publish Date: August 2024
Cincinnati Children’s one of four centers sharing experiences after implementing training changes
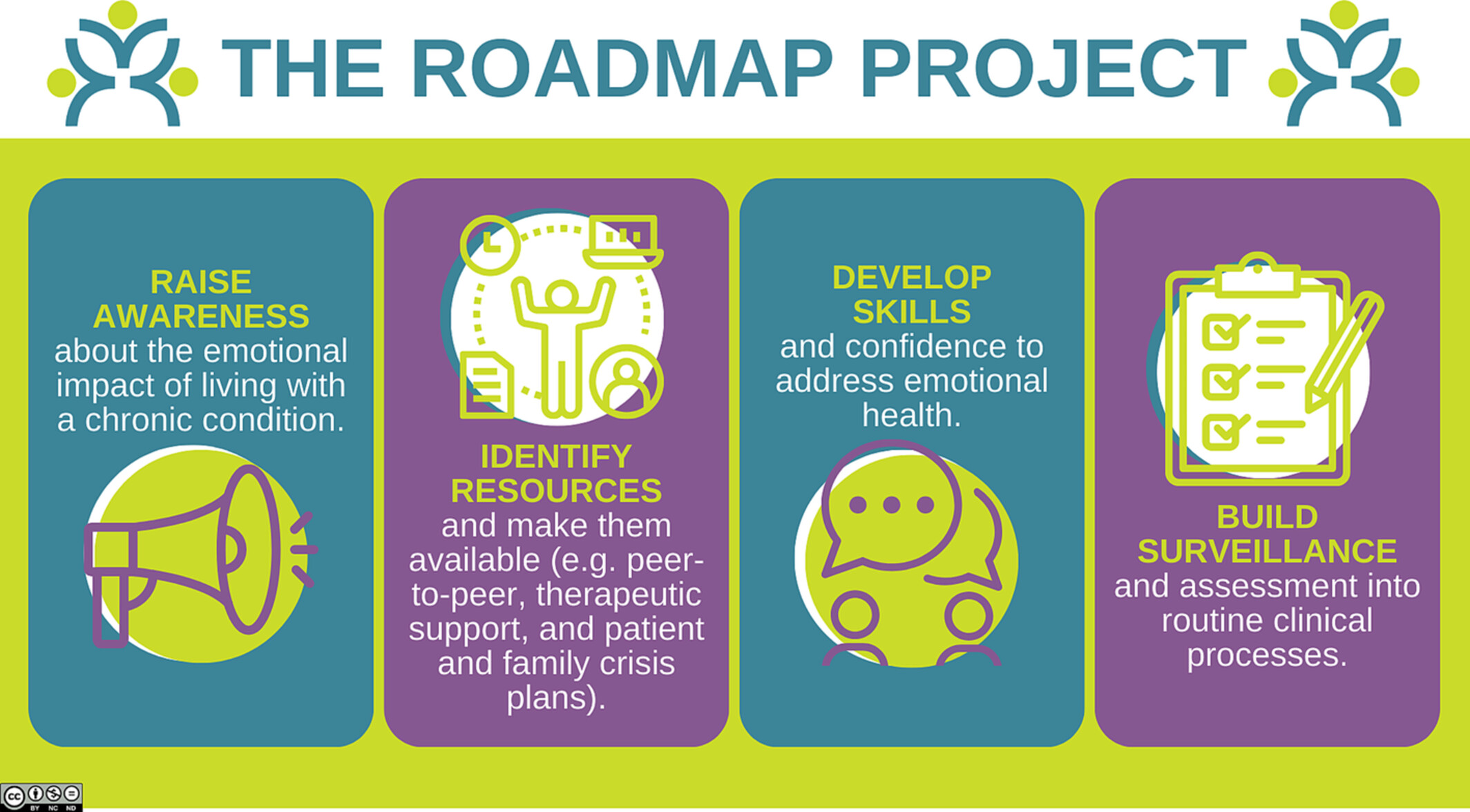
Children with chronic medical conditions and their families have significant emotional health concerns, yet pediatricians report that they are often ill-equipped to address these needs. To support pediatricians in addressing emotional health as part of routine care, the American Board of Pediatrics launched The Roadmap Project in 2018.
Now, Cincinnati Children’s and three other institutions that recently implemented Roadmap Project tools and strategies into their pediatric training programs have shared their experiences in The Clinical Teacher, a journal for clinicians who teach and others who provide education in healthcare settings.
“Addressing the emotional health of patients with chronic conditions in the clinical space has not traditionally been part of the clinician’s scope of practice and requires a cultural shift in addition to educational interventions,” says co-author Sue Poynter, MD, MEd, pediatric residency program director at Cincinnati Children’s.
Educators from Cincinnati Children’s, MedStar Georgetown University Hospital, Nationwide Children’s Hospital, and the University of North Carolina Children’s Hospital tested integrating Roadmap resources into their programs in different ways, either by incorporating them into existing educational structures or embedding them into the clinical workplace. Each team selected a clinical or educational setting and applied Roadmap resources of their choice to improve selected key drivers.
Survey confirms positive change
The Cincinnati Children’s team, led by co-author Lori Herbst, MD, and advised by Poynter, incorporated Roadmap tools into the curriculum for residents rotating on the complex care inpatient service.
They added emotional health ‘check-ins’ with patients and families during daily bedside rounds (e.g. “how are you doing?”), which was a distinct change to typical rounding primarily focused on medical management. They also tested a modification to provider handoffs adding an emotional health ‘system’ into standard weekly patient handoffs to oncoming clinical teams.
The team surveyed parents through text message and learned that 58% of those responding confirmed that emotional health had been addressed during the hospital admission.
Tools easy to adapt
The educators found that the tools were easily adaptable to multiple educational and clinical environments and learner levels. Despite differences in implementation, all approaches were effective in meeting Roadmap objectives for pediatric trainees: increasing clinician awareness of emotional health needs of patients with chronic conditions and their families and increasing skills and confidence in supporting those needs.
In addition, they found that although learning in a traditional education program can improve an individual’s practice, educating clinical teams together may be more impactful for prompting sustainable behavior change in clinical practice.
Shared lessons learned from these institutions led to improvements in training materials, greater involvement of patient families in trainee educational activities, and creation of a new module on the additional burdens of chronic conditions on families of minority racial groups.
About the study
Senior author Carole Lannon, MD, MPH, a member of the James M. Anderson Center for Health Systems Excellence, is the principal investigator of the national Roadmap Project. Co-authors from Cincinnati Children’s also included Christine Schuler, MD, MPH, Division of Hospital Medicine.
The project is funded by the American Board of Pediatrics Foundation and the David R. Clare and Margaret C. Clare Foundation.
| Original title: | Integrating education for clinical practice change |
| Published in: | The Clinical Teacher |
| Publish date: | August 2024 |
Research By



Identifiable gaps in health outcomes piqued my research interests. I now work with patients, families, clinicians and researchers to improve care and outcomes for children and families using learning health networks. These networks, used for improvement and research, can accelerate population health outcomes at scale.