Innovation in Action: How Cincinnati Children’s Brought an Improvement in Anesthesia Care to Life
Post Date: October 24, 2023 | Publish Date:

It takes an average of 17 years for medical discoveries to move from publication to the bedside, according to the National Academy of Medicine. However, by tapping into product development and commercialization expertise at Cincinnati Children’s, a team of innovators needed just five years to convert a nurse practitioner’s concept for reducing anesthesia induction anxiety into a licensed software product now used by more than 160 institutions in eight countries.
In 2014, Abby Hess was working as a nurse practitioner at Cincinnati Children’s and pursuing a Doctor of Nursing Practice degree. The DNP degree was created to prepare nurses for leadership positions where they can translate research into practice to improve patient outcomes. The degree requires a capstone project that focuses on implementing practice changes that solve real-world clinical problems. It did not take long for Hess to identify a need.
A daily part of Hess’ role included working collaboratively with patients, families and other clinical team members to develop a plan to address pediatric anxiety before surgery. She quickly realized that after developing a plan to reduce anxiety, there was no clinical documentation or communication regarding the patient’s anxiety behaviors during anesthesia induction.
“Without this documentation, there was no way to know whether preoperative interventions were actually effective in reducing anxiety in the operating room. Additionally, if the patient came back for a subsequent surgery, there was no documentation to help guide the plan for anxiety reduction.”
Hess reviewed existing scientific research and found that there was no simple clinical practice tool for documenting pediatric patients’ behavioral response to anesthesia inhalation induction. So, she decided to create one.
CIBA Version 1
As a busy nurse practitioner, Hess knew that for any new tool to be impactful, it would need to be evidence-based, succinct, clinically meaningful and easy to use. She worked with Anna Varughese, MD, MPH, an anesthesiologist and quality outcomes researcher at Cincinnati Children’s, to develop a simple, evidence-based electronic tool named the Child Induction Behavioral Assessment (CIBA).
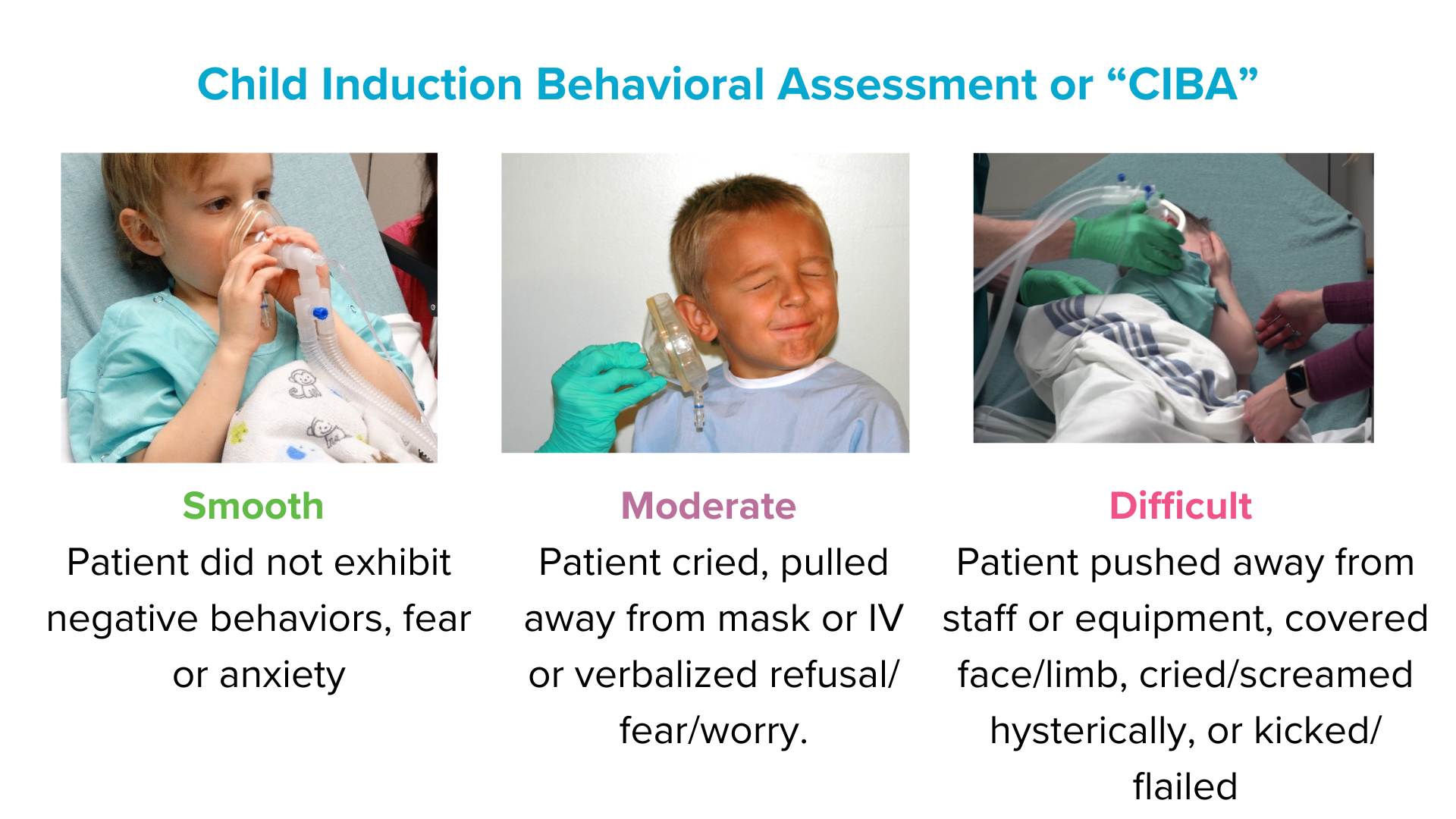
The CIBA tool asked anesthesia providers if the induction was smooth (calm and cooperative), moderate (for example, cried, pulled away or expressed fear) or difficult (for example, pushing away and covering face, screaming).
The Cincinnati Children’s team implemented the tool, made modifications, and found it was very effective at assessing perioperative strategies by comparing the intervention to the patient outcome. Hess and her team published their findings in June 2018 in the Journal of PeriAnesthesia Nursing, in hopes that others might benefit.
As with any new tool, validation is important. However, validation is a process that takes time and money to achieve. In the face of this hurdle, Hess collaborated again with Varughese, along with biostatisticians Monir Hossain, PhD, and Lili Ding, PhD, and neuroscientist Bob Coghill, PhD. With support from her collaborators, Hess wrote her first research grant proposal, which secured an internally funded Anesthesia Innovation and Pilot Award.
These funds, offered through the Department of Anesthesiology, covered the salary for two part-time clinical research coordinators, Lauren Hill, MSN, and Bobbie Stubbeman, BS, who completed the data collection for 384 enrolled patients. Hess and colleagues validated CIBA in a two-year study published in February 2020 in Anesthesia and Analgesia.
CIBA Version 2
A few weeks after publication, they received a call from Clyde Matava, MD, MMEd, MHSC, associate chief of Perioperative Services for Bioinformatics at the Hospital for Sick Children in Ontario, Canada. As it turns out, Matava had already been working with Epic, a widely used electronic health record platform, on creating a similar assessment tool that also included standardized interventions and future recommendations. Matava was looking for a validated tool that could be incorporated into the larger standardized pediatric induction assessment, and CIBA seemed to fit the bill.
Even though Hess didn’t know how to incorporate this tool into Epic at the time, she didn’t let that stop her. She tapped into Cincinnati Children’s Innovation Ventures, the institution’s technology transfer office, which worked with Hess to license CIBA to Epic so that it could be used by Matava as well as other Epic users around the world.
“Innovations that are validated and helpful internally are not necessarily easy to adopt or commercialize externally,” says Justin Levy, Director of Portfolio Management, Innovation Ventures. “In order to make the innovation attractive to a licensee who will in turn take it to market, intellectual property protection and iteration with input from patients and external partners may be necessary.”
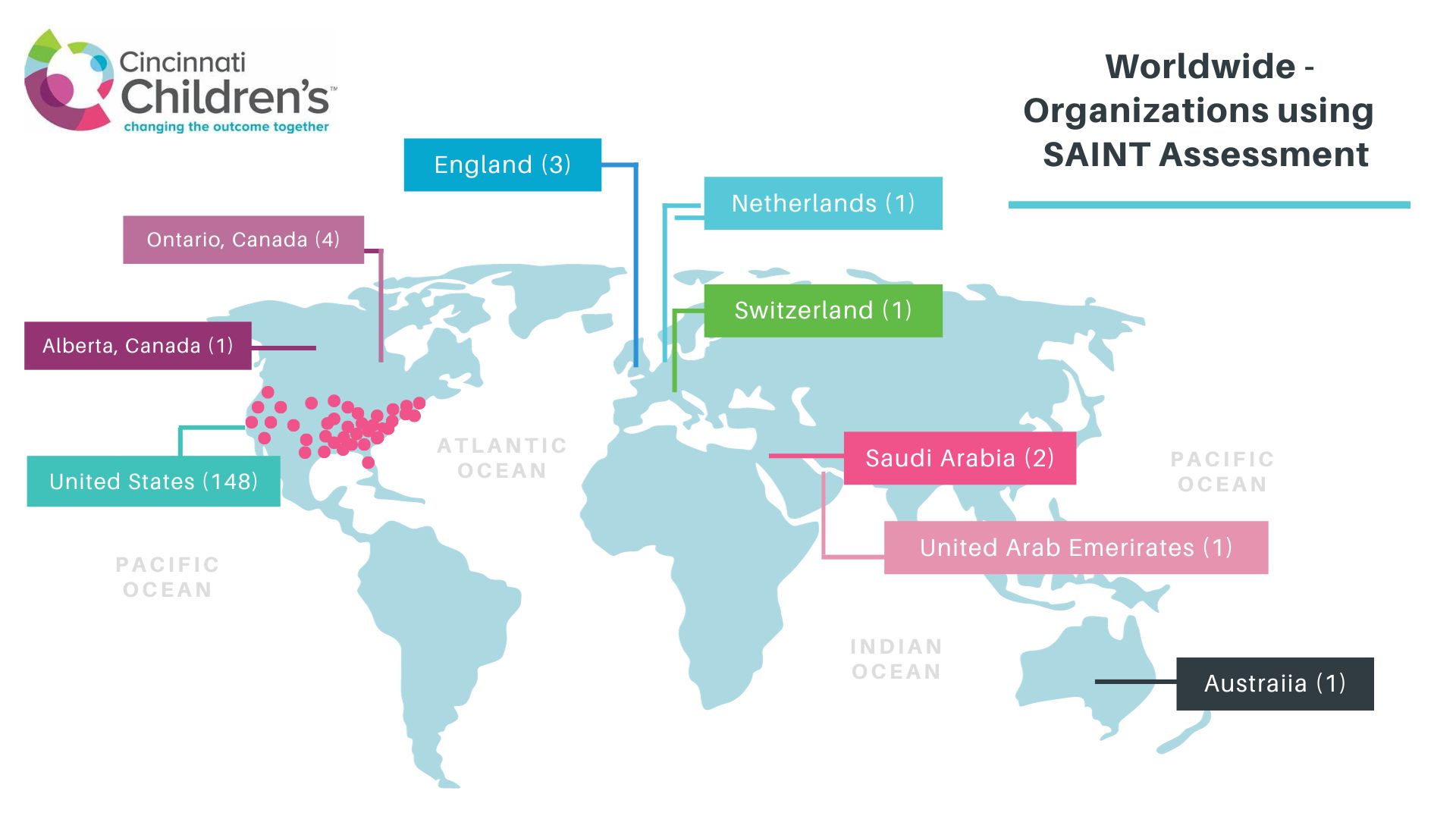
Now, the CIBA tool is incorporated into a Standardized Anesthesia Induction Tool (SAINT), which is part of the foundation build of Epic. This essentially means that any hospital using Epic has access to incorporate this tool into its routine clinical documentation. It is currently being used in 162 organizations and eight countries around the world.
Research continues
The collaboration with the Hospital for Sick Children did not end there.
“We recognized that there were significant differences in what interventions are used for anxiety reduction,” Hess says. “For example, hospital staff reported that administration of anxiety medication before surgery ranged from 10% to 90% in hospitals caring for similar patient populations.”
Now, Matava and team are conducting a multinational research study, in which Cincinnati Children’s plays a key role. The study plans to include over 75,000 kids – and for the first time ever, it allows the users to look retrospectively at the different practices that were implemented and their relationships to outcomes. With their team of analysts, the Hospital for Sick Children is analyzing the data. The findings will be shared in late 2023.
“Because of the vast resources available at Cincinnati Children’s, I was able to find collaborators to help me take an evidence-based idea to implementation, validation, licensing, and back to research to further improve practice,” Hess says.
While the research portions of the project required years to accomplish, several other critical milestones were reached relatively quickly.
- The resources within Cincinnati Children’s enabled this tool to go from ideation to initial implementation within around six months.
- Within less than a year, Hess’ initial validation grant was written and funded internally by the Department of Anesthesiology,
- Meanwhile, building the collaboration with the Hospital for Sick Children and completing the licensing for use in Epic took only several months to accomplish.
Next steps
Future steps in the project aim to improve clinical practice in multiple ways. In addition to using the retrospective data analysis described above, Cincinnati Children’s will be using a new tool that is readily available on Epic called the Slicer Dicer. This tool allows clinicians to access Epic data and build reports themselves.
“Many people do not know about this Epic feature, but it lets you almost immediately pull and analyze electronic health record data from Epic using a variety of parameters,” Hess says. “You can look across different populations or clinical locations and quickly see how interventions and outcomes may differ. This provides valuable insights for future quality improvement initiatives.”
Accessing clinically relevant data used to take many months, and modifying existing reports was often quite cumbersome. With Slicer Dicer, accessing and modifying reports can take just hours to minutes.
From acquiring department level grant funding for research and validation, to working with Innovation Ventures to license the technology to Epic, the support Cincinnati Children’s supplies is evident. The synergy that created this simple, usable tool attracted the attention of research partners with the ability to scale it for research and practice improvement. This tremendous effort on the part of Hess and her colleagues demonstrates that with the will to do so, Cincinnati Children’s employees can speed up the transfer of novel knowledge to improve the outcome together.