Engineered Organoids Might Serve as Bridge to Liver Transplantation in Severe Jaundice
Research By: Takanori Takebe, MD, PhD | Hasan Al Reza, PhD
Post Date: October 23, 2023 | Publish Date: Oct. 12, 2023
Experts at Cincinnati Children’s report another beneficial use case for lab-grown human organ tissues
Many parents are familiar with the risk some newborns face from jaundice, a condition marked by a yellowing of the infant’s skin because the liver does not remove enough bilirubin from the bloodstream. In most cases, exposing the newborn to increased amounts of sunlight, either naturally or artificially, takes care of the temporary problem.
But for a small number of newborns with jaundice, sunlight isn’t enough. In fact, about 114,000 children worldwide die each year because their livers never remove enough bilirubin. For these children, receiving a liver transplant has been their main hope for living into adulthood.
Now, the emerging field of organoid medicine suggests a new approach may improve survival chances for children with difficult-to-treat jaundice, including serving as a potential “bridge” to help children live long enough to receive a full organ transplant.
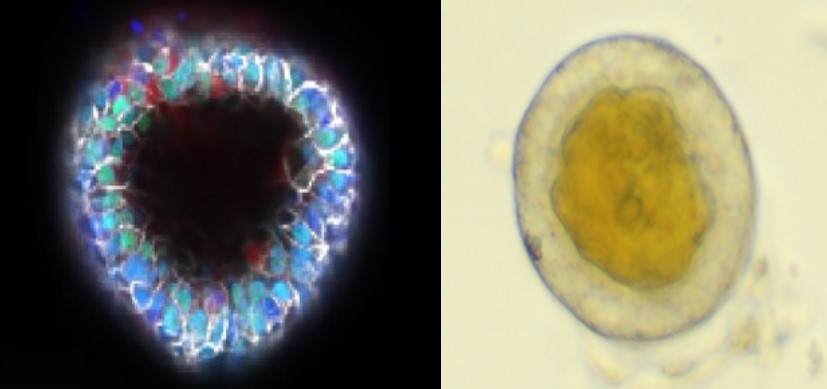
In a series of human organoid and rodent model experiments, a research team led by first author Hasan Al Reza, PhD, and senior author Takanori Takebe, MD, PhD, reports that human liver organoids can be augmented to improve how they filter out bilirubin. In rodents, injecting these tiny chunks of functioning organ tissue into a dysfunctional liver can sharply reduce jaundice symptoms and potentially delay the need for an organ transplant, according to findings published Oct. 12, 2023, in Stem Cell Reports.
“These early-stage findings are important because the available supply of donated organs for liver transplantation does not meet the number of patients in need,” Takebe says. “It now appears possible for liver organoids to support liver function without necessarily growing a full-sized replacement organ.”
Journey started with a family supporting science
The research team is particularly interested in whether engineered organoids can help people with Crigler-Najjar syndrome (CNS), a form of hyperbilirubinemia caused by a mutation in the UGT1A1 gene. The condition affects about one in 1 million live births.
This study traces its roots to a Japanese man, now 24, who was born with severe jaundice that did not respond to phototherapy and other treatments. At age 5 he received a partial liver transplant from his mother. This man’s tissue samples helped the team make its breakthrough.
“We were able to generate a stable line of pluripotent stem cells that carried the UGT1A1 mutation, which allowed us to conduct more analysis,” Reza says. “From there, we were successful at engineering an organoid that could overcome the gene mutation for a meaningful length of time.”
Mouse gene provides a boost
The new organoid was gene-edited to include a mouse gene that makes these organoids synthesize their own vitamin C to manage bilirubin levels more efficiently. Humans lack a similar gene.
When transplanted into rats with severe jaundice, the engineered organoids restored bilirubin control to near-normal levels. However, this function began to decline after 40 days and dropped below clinical benefit by about 60 days.
Much more research will be needed to further prepare this advance for human clinical trials, co-authors state, including addressing apparent rejection of the engineered organoids. More study also would be needed to determine if other liver conditions might be improved via this type of miniature organoid transplant.
“Nearly two months of improved function in an animal model is a significant step forward,” Takebe says. “If we can develop more robust versions of this therapy that also reduce the rejection risks, organoid transplantation might someday provide more time for finding a suitable donor organ.”
About this study
This study was funded by several sources, including the National Institutes of Health (DP2 DK128799-01 and UG3/UH3 DK119982), a PHS Grant (P30 DK078392) and multiple grants from the Japan Agency for Medical Research and Development. Funding sources also included the Cincinnati Children’s Research Foundation, the Cincinnati Center for Autoimmune Liver Disease, the Falk Transformational Awards Program, the Takeda Science Foundation, and the Mitsubishi Foundation. The authors declare no competing interests.
| Original title: | Synthetic augmentation of bilirubin metabolism in human pluripotent stem cell-derived liver organoids |
| Published in: | Stem Cell Reports |
| Publish date: | Oct. 12, 2023 |
Research By

With a major focus on foregut- and midgut-derived systems, our lab aims to contribute to human health by establishing new therapies especially for treating pediatric intractable disease.






