How to Cool Neighborhood Hospitalization Hotspots
Research By: Andrew Beck, MD, MPH | Robert Kahn, MD, MPH | Uma Kotagal, MBBS, MSc
Post Date: September 4, 2019 | Publish Date: Sept. 3, 2019
Through a mix of data-driven insights and layers of teamwork, a pediatric medical center and its community partners have demonstrated that hospitalization rates can be reduced among children living in neighborhoods with high rates of illness and poverty.
According to a study published Sept. 3, 2019, in Health Affairs, experts at Cincinnati Children’s led a series of interventions that significantly reduced hospitalization rates in Avondale and Price Hill, two neighborhood in Cincinnati that have struggled for years with high rates of asthma, preterm births and other childhood illnesses.

In 2015, the Cincinnati Children’s team defined its goal: to reduce the inpatient bed-day rate for children from Avondale and Price Hill by at least 10 percent by June 30, 2020.
They overachieved.
The Health Affairs study reports that the inpatient bed-day rate for the two target neighborhoods decreased by 18 percent by June 2018—well ahead of schedule. Total hospitalizations also decreased by 20 percent. Meanwhile, other demographically comparable neighborhoods experienced no reduction in hospitalization rates.
Thanks to this work, children from these neighborhoods were able to spend hundreds more healthy days at school and being active at their homes, instead of receiving hospital care, the co-authors state.
How were hospitalization rates reduced?
Improvement efforts began in July 2015, by assembling a team of inpatient and outpatient medical providers, social workers, parents and community partners, including the Legal Aid Society of Greater Cincinnati and others.
Interventions included optimizing chronic disease management practices at the hospital and in neighborhood health clinics; an increased focus on hospital-to-home care transitions; and mitigating social risks in achievable ways. All of it based on actionable, real-time data.
Much of the community engagement work in this project was encouraged and coordinated through the All Children Thrive Learning Network, launched several years ago by a network of community partners.
The reduced hospitalizations also reflect a deep institutional commitment to improving child health in the hometown of Cincinnati Children’s, one of the nation’s top pediatric care and research centers. Many of the methods used to achieve these successes have been championed for years by Uma Kotagal, MBBS, MSc, a renowned leader in health care quality improvement.
Kotagal helped launch the James M. Anderson Center for Health System Excellence at Cincinnati Children’s, which has supported a wide range of population health improvement projects. The hospitalization project reflects the center’s goals, including striving to assure that families are partners in improvement efforts and well-equipped to manage chronic illnesses at home. The Center also has a long track record of working with community agencies to remove barriers to health and of working within the complexities of an academic medical center to build teamwork and adopt evidence-based best practices.
Colleagues Robert Kahn, MD, MPH, study first author Andrew Beck, MD, MPH, and others at Cincinnati Children’s have been working with Kotagal for years. They too have track records of community impact.
Kahn and Beck have worked with city officials and the Legal Aid Society to improve unhealthy conditions in rental housing. Beck also was part of a team at Cincinnati Children’s that led an ambitious community-wide asthma care improvement project that slashed hospital return visits within 30 days of discharge among Medicaid-insured children by 41 percent.
Some of the admissions reductions cited in the Health Affairs study trace back to that asthma project. Now, children routinely leave the hospital with a supply of asthma medications in-hand, not just a prescription to fill later. Some families also get medications delivered to their homes or schools. Thanks to improved use of electronic care records, increased involvement of school nurses, and other steps, once-scattered asthma care services have become much more coordinated.
The new study reports that similar efforts have been applied to other chronic conditions, including diabetes.
Other co-authors of the Health Affairs study were: Srikant Iyer, MD; Kristy Anderson, LISW-S; and analysts Kate Rich and Stuart Taylor.
“We have pushed our health care system and community to be accountable to populations and neighborhoods that are disproportionately affected by medical and social challenges. We have made early progress toward keeping children out of the hospital. We now seek to take what we have learned and push toward scale and spread.”
—Co-authors, Health Affairs study, published Sept. 3, 2019.
Care huddles make a difference
When children from the two neighborhoods were admitted to the hospital, the intervention team was alerted. This allowed huddles of physicians, nurses, social workers, community engagement consultants, and teachers from school services to form and look for opportunities to prevent future hospitalizations. Their work has ranged from catching up on overdue immunizations to making sure families arrive for follow-up appointments to helping students keep up with schoolwork.
In the community, parents have joined groups organized through All Children Thrive that have focused on issues ranging from hand hygiene to housing rights. In fact, a community meeting that discussed local asthma rates helped lead to action to mitigate an asthma “hot spot” in a neighborhood building complex.
What’s next?
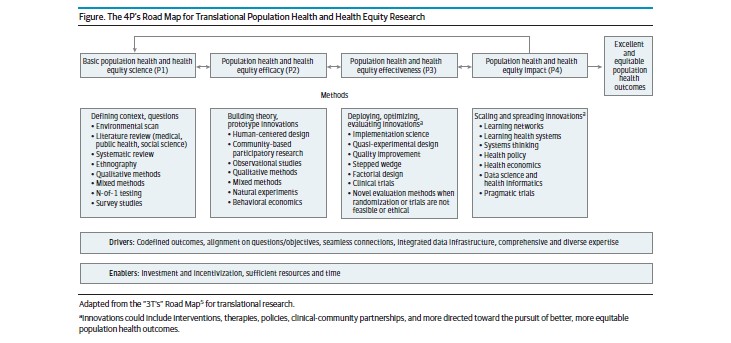
While many of the methods used to reduce child hospital admissions in Cincinnati can be applied in other cities, the study co-authors state that the mix of health issues and the array of available community partners can differ. Each local solution must be crafted according to local needs.
Even so, the study also raises potential regional, state and national policy issues. For example, the study suggests that health improvements could be scaled up faster if more hospitals were paid, at least in part, according to population health improvement metrics rather than primarily fee-for-service models.
Likewise, co-authors suggest that private insurers and government payers should consider supporting reimbursement for organizations, like Legal Aid and others, that traditionally have not been considered health organizations but still play key roles in accelerating population health improvements.
See related coverage in Modern Healthcare.
See commentary in JAMA Forum: Moving to Action on Place-Based Health
| Original title: | Cooling The Hot Spots Where Child Hospitalization Rates Are High: A Neighborhood Approach To Population Health |
| Published in: | Health Affairs |
| Publish date: | Sept. 3, 2019 |