Electronic Health Records and Machine Learning Illuminate Racial Disparities for Asthma Risk
Research By: Tesfaye Mersha, PhD
Post Date: March 10, 2021 | Publish Date: Nov. 9, 2020
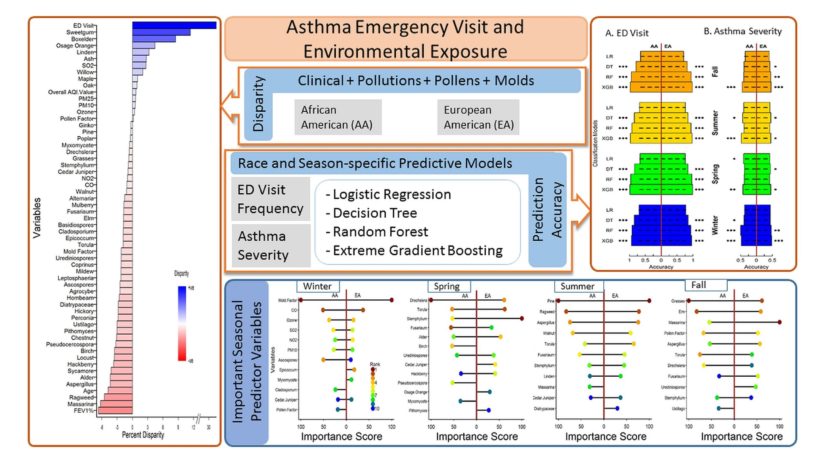
Seasonal factors can make any person with asthma more likely to visit the emergency department (ED). Yet if that person is of African American descent, they are even more likely to visit the ED.
What are the environmental exposures driving these season- and race-specific visits, and how can we better understand them to improve patient care?
By combining data from the electronic health record with machine learning techniques, researchers at Cincinnati Children’s unraveled the impact of environmental factors on racial disparities in asthma health care. Their findings were published Nov. 9, 2020, in the Journal of Asthma.
Investigating a Public Health Issue
Racial disparities in medical care continue to be a pressing public health issue—and asthma care is no exception.
“As the COVID-19 pandemic shows, there are a lot of disparities that need addressing,” says corresponding author Tesfaye Mersha, PhD, of the Divisions of Asthma Research and Global Health. “Investigation into the various health-related racial disparities allows researchers to unravel risk factors driving the disparities and make better decisions.”
After observing trends in asthma ED visits, researchers wondered—how do season-specific environmental exposures impact patients differently based on race? During the COVID-9 pandemic, answers to this question may be more important than ever. The greater the amount of time people spend at home, the higher their exposure to possible untreated residential mold.
To address this problem, researchers examined data from 42,375 individuals identified in electronic health records. Various data types helped to give a more complete picture of each patient. These included demographic (race, age, gender, insurance), clinical (smoking status, ED visits, FEV1%), and environmental exposures data (mold, pollen, pollutants) from the Greater Cincinnati region.
After splitting the dataset by race and seasons, researchers used machine learning techniques to create predictive models for asthma severity and ED visit frequency. This approach allowed the team to gain better insights on how these factors interact.
Among the individuals studied, researchers observed significant differences in ED visits and FEV1% based on race. For those of African American descent, ED visits were 32% higher and FEV1% value was 6.4% lower compared to those of European American descent. For both groups, pollen factor and pollution were the key variables for asthma, whereas age and cigarette smoking increased risk regardless of seasonal factors.
Improving Decisions for Asthma Care
As the asthma disparities highlighted in the study show, there is a need to address these disparities through key predictors—namely socio-economic status, particulate matter, and mold.
In the clinical setting, physicians and other health professionals can pay close attention to baseline differences in environmental exposure regarding asthma. With greater awareness of race- and season-specific triggers, care providers are better able to determine the likelihood of a higher load of asthma admissions on a given day or season.
For patients and families, knowledge of these disparities can help determine when to take extra precautions. When pollen count and pollution levels are high, they may consider carrying a rescue inhaler. At-risk individuals may also want to learn more about avoiding mold development in homes.
Within communities, a focus on multi-prong intervention strategies can help tackle the health issues of asthmatics, reducing the disparities affecting at-risk populations. Public health officials can leverage this research to make better decisions and policy incentives to tackle the molds and pollens that disproportionately affect those of African American descent.
As a step toward achieving these goals, researchers plan to develop localized models based on neighborhood. Greater localization could produce results with more targeted, place-specific information.
“This may push for the creation of public health tools tailored to minimize the racial disparities on asthma health for racially diverse population centers like the Cincinnati metropolitan area,” says Mersha. “We believe that health disparities are modifiable and preventable.”
| Original title: | Unraveling racial disparities in asthma emergency department visits using electronic healthcare records and machine learning |
| Published in: | Journal of Asthma |
| Publish date: | Nov. 9, 2020 |
Research By