Clinical Trial Begins for Novel Natural Killer Cell Therapy
Post Date: January 5, 2024 | Publish Date:
Study to Focus on Adolescents and Young Adults with Relapsed or Refractory Acute Myeloid Leukemia
Cincinnati Children’s is one of only a few centers in the nation to test a novel therapy that uses cytokine-induced memory-like natural killer (CIML-NK) cells from haploidentical donors to treat acute myeloid leukemia (AML). This study is open to patients ages 12 to 45 years with relapsed or refractory AML who have not undergone bone marrow transplantation.
The research team infused the study’s first patient in May 2023, a significant technical, quality assurance and manufacturing achievement. The process took approximately three weeks and involved about 30 people from the Cincinnati Children’s bone marrow transplantation team, Cellular Manipulations and Diagnostic Immunology Laboratories, and the Hoxworth Blood Center.
Study is Now Open to Patients 12 and Above
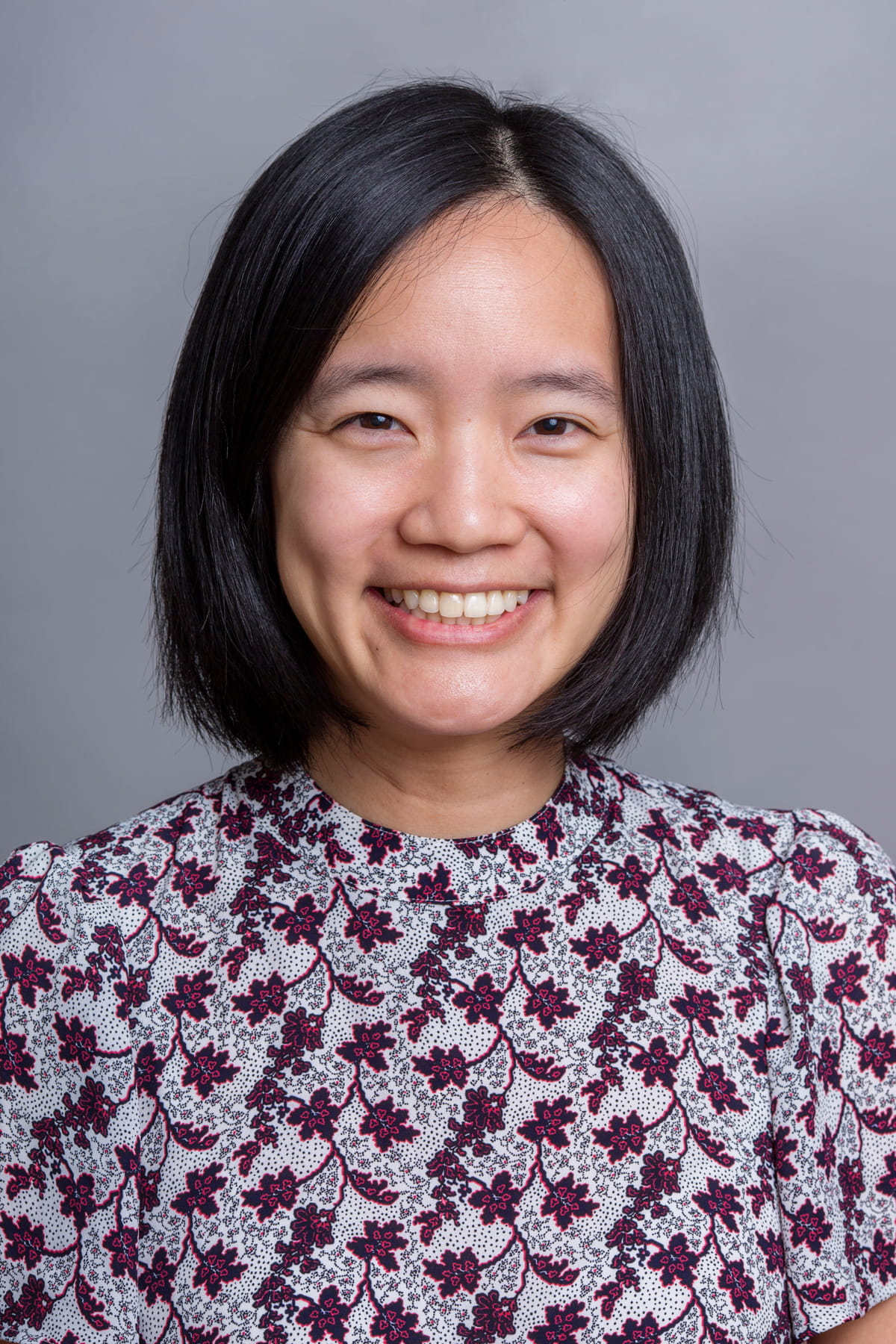
“This was the first time we manufactured this cell therapy for and treated a patient with this therapy, and we were thrilled our process went as smoothly as it did, with no ill effects,” says principal investigator YunZu Wang, MD, a pediatric hematologist/oncologist with the Division of Bone Marrow Transplantation and Immune Deficiency.
“We are especially excited that, in light of how well our first infusion went, the U.S. Food and Drug Administration has allowed us to lower the minimum age of study participants from 18 to 12 years old, giving us the opportunity to offer the therapy to pediatric patients.” —YunZu Wang, MD
The team’s main challenge now is getting the word out about the therapy and encouraging cancer specialists around the country to refer patients who might meet eligibility guidelines.
NK Cell Therapy: A Better Option for AML Patients?
Most people associate cellular therapy with chimeric antigen receptor (CAR) T-cell therapy for acute lymphoblastic leukemia (ALL), which can be effective but also is associated with risks that include cytokine release syndrome and neurotoxicity.
“To date, cellular therapy options for patients with AML have been limited by toxicity from the cellular therapy,” Wang says. “NK cell therapy may be a better option for them. Prior research studies suggest that the incidence of these complications is much lower when NK cells, including these memory-induced NK cells, are used.”
T cells and NK cells are both lymphocytes but have one critical difference when using them for cancer-fighting purposes. To recognize and kill cancer cells, T cells must be “taught” by previous exposure or be genetically modified to recognize cancer cells. In contrast, NK cells can recognize cells that are not “self” and kill them on the first interaction.
The Haploidentical Advantage
The study protocol requires that the NK cells come from a haploidentical donor, such as a parent or sibling. “In previous retrospective studies of patients with AML who had a bone marrow transplant, those with a slight NK cell mismatch experienced a better treatment response and had a lower incidence of graft-versus-host disease compared to those who did not have NK cell mismatch with their bone marrow transplant donor,” Wang says.
When a patient enrolls in the study, the research team tests potential haploidentical donors to identify the best candidate. Patients begin a reduced-intensity chemotherapy regimen to temporarily destroy lymphocytes so that the patient’s own lymphocytes do not reject the donor NK cells.
Hoping to Improve on Dismal Outcomes
After the patient completes chemotherapy, the donor’s blood cells are collected and processed at the Cincinnati Children’s Cell Manipulations Lab. The CIML-NK cells are infused the day after collection. The patient remains hospitalized while their cell counts recover. The care team repeats a bone marrow test after a month, and patients in remission can go straight into transplant as a curative option.
Finding more effective therapies for recurrent and refractory AML is critically important. Current treatment outcomes result in a dismal overall five-year survival rate of 35%.
“Half or more of patients with recurrent or refractory disease never achieve remission and are not offered a bone marrow transplant,” Wang says. “Those who make it to transplant have been exposed to so much chemotherapy that they are at high risk for long-term organ effects.”
“We strongly believe that the toxicity of our experimental therapy is very low compared to standard salvage AML therapy,” Wang adds. “If the regimen is found to be safe and effective in adolescents and young adults, we hope to offer the therapy to even younger patients in the future.”