Airway Remodeling Creates Susceptibility to Frequent Asthma Exacerbations in Children
Research By: Kieran Phelan, MD | Gurjit Khurana Hershey, MD, PhD
Post Date: March 12, 2023 | Publish Date: Mar 12, 2023
Asthma Research | Top Scientific Achievement

Asthma is a common allergic respiratory disease found in both children and adults. Yet the mechanisms underlying asthma pathogenesis and exacerbation frequency have been understudied, despite the high healthcare costs and morbidity rates associated with frequent asthma exacerbators in both populations.
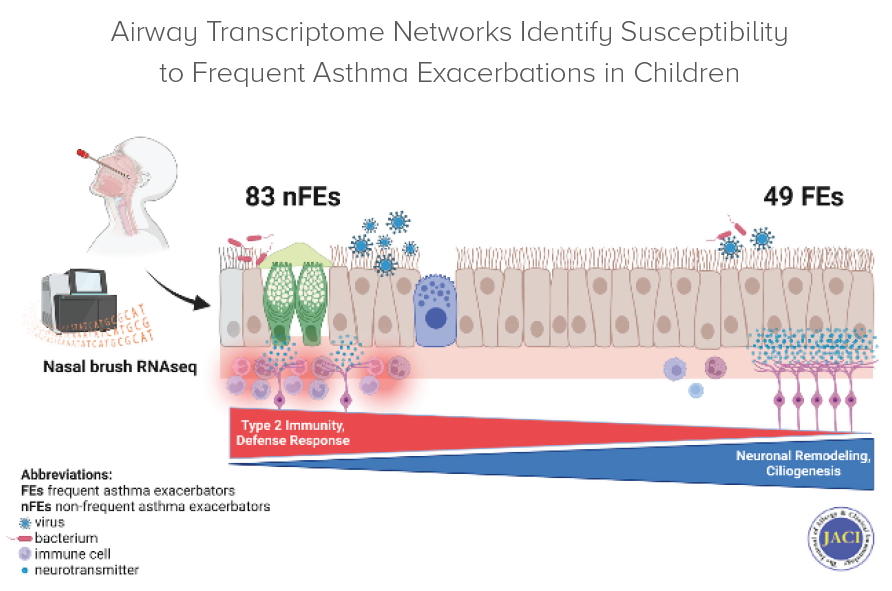
In a study led by first author Kieran Phelan and senior author Gurjit “Neeru” Khurana Hershey, MD, PhD, researchers for the first time implicated the nervous system as having a role in recurrent exacerbation pathology in children with asthma. They also highlighted frequent asthma exacerbators—patients hospitalized two or more times in a year for a severe asthma event—as a biologically distinct endotype in children.
For the study, researchers studied biospecimens, including nasal epithelial cells and blood, and health outcomes data collected by the Ohio Pediatric Asthma Repository from 132 pediatric asthma exacerbators—both frequent and non-frequent—who were treated at one of Ohio’s major children’s hospitals, including those in Cincinnati, Cleveland, Columbus and Dayton. Their goal was to identify the clinical and molecular features specific to children prone to recurrent severe asthma exacerbations, also known as frequent exacerbators (FEs).
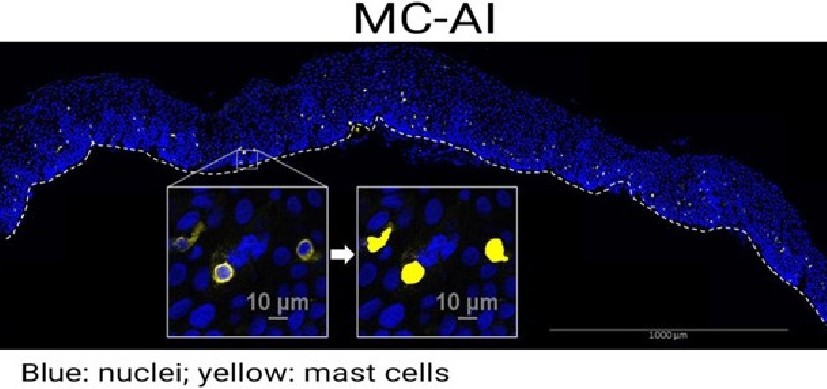
Among their findings, researchers discovered that FEs displayed a unique increase in gene signatures associated with nervous system processes, while the airways of non-FEs were characterized by the expression of allergic inflammation previously known to be involved in asthma.
The study’s results suggest that more frequent asthma exacerbations don’t lead to more severe exacerbations. Instead, repeated exacerbations result in neuronal airway remodeling that prime it to react the same way it has in the past.
“Our findings highlight fundamental differences in these exacerbations and suggest that therapy targeting neuronal pathways may be necessary to adequately prevent and/or treat frequent exacerbations,” Khurana Hershey says.
More 2023 Research Highlights
Chosen by the Division of Asthma Research
DeVore SB, Stevens ML, He H, et al. Novel role for caspase recruitment domain family member 14 and its genetic variant rs11652075 in skin filaggrin homeostasis. J Allergy Clin Immunol. 2022;149(2):708-717. doi:10.1016/j.jaci.2021.07.003
Correa-Agudelo E, Beck AF, Mersha TB. Racial differences in emergency encounters related to pediatric allergic diseases during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2023;11(7):2232-2234.e1. doi:10.1016/j.jaip.2023.04.007
Brandt EB, Ruff BP, Filuta AL, Chang WC, Shik D, Khurana Hershey GK. Thymic stromal lymphopoietin rather than IL-33 drives food allergy after epicutaneous sensitization to food allergen. J Allergy Clin Immunol. 2023;151(6):1660-1666.e4. doi:10.1016/j.jaci.2023.02.025
Gautam Y, Mersha TB. Leveraging genetic ancestry to study severe asthma exacerbations in an admixed population. Thorax. 2023;78(3):220-221. doi:10.1136/thorax-2022-219459
View more discoveries from 50 research divisions and areas
Return to the 2023 Research Annual Report main features
| Original title: | Airway transcriptome networks identify susceptibility to frequent asthma exacerbations in children |
| Published in: | The Journal of Allergy & Clinical Immunology |
| Publish date: | Mar 12, 2023 |
Research By

My lab combines epidemiologic, basic, translational and clinical research approaches to answer fundamental questions related to childhood asthma, atopic dermatitis, food allergy and allergic rhinitis.