Addressing the Mental Health Crisis Facing Our Youth: Cincinnati Children’s Takes a Proactive Approach
Research By: Michael Sorter, MD | Lori Stark, PhD | Tina Cheng, MD, MPH | Tracy Glauser, MD | Jessica McClure, PsyD | John Pestian, PhD, MBA | Kate Junger, PhD
Post Date: May 30, 2023 | Publish Date: May 13, 2023
Leaders describe multiple steps taken plus work in progress to help children before they need psychiatric hospital care
As the nation grapples with a childhood mental health crisis, leaders at Cincinnati Children’s are sharing details of a years-long ongoing effort to move care further “upstream” so that more children can receive help before their problems become severe.
These efforts have involved more than $100 million in facility improvements, sweeping practice changes that affect dozens of community pediatric offices, school health services and primary care clinics, plus deep investment in far-reaching research involving one of the world’s largest supercomputers to create a novel mental health early warning system.
Their work is detailed in a report published online May 12, 2023, in The Journal of Pediatrics.
“Our blue-sky goal is to eliminate pediatric suicides by 2033,” says the study’s corresponding author Tina Cheng MD, MPH. “To achieve that goal, we are moving away from a primarily reactive approach to care to a much more proactive approach. The work started here more than six years ago is building a strongly integrated system of care that focuses on early prevention while providing truly innovative ways to serve children and families in crisis.”
Cheng, a nationally known figure in pediatric population health research and policy, is director of the Cincinnati Children’s Research Foundation, chair of Pediatrics at the University of Cincinnati College of Medicine and chief medical officer for the health system.
First authors on the paper include key leaders in a systemic transformation of mental health care at Cincinnati Children’s: Lori Stark, PhD, director of Behavioral Medicine and Clinical Psychology, and Michael Sorter, MD, director of Child and Adolescent Psychiatry; Tracy Glauser, MD, associate director of the Cincinnati Children’s Research Foundation; Jessica McClure, PsyD, medical director for population behavioral health; psychologist Katherine Junger, PhD, associate medical director for population behavioral health; and John Pestian, PhD, MBA, director of the Computational Medicine Center.
A Deep Crisis
Cincinnati Children’s provides more mental health care services than any other pediatric hospital in the U.S., including a 130-bed psychiatric hospital, extensive outpatient therapy services and deep ties with local schools and community organizations. Yet, much like the rest of the nation, the pediatric emergency department here has been overwhelmed by demand. The surge was occurring before the COVID-19 pandemic but has only grown more intense since.
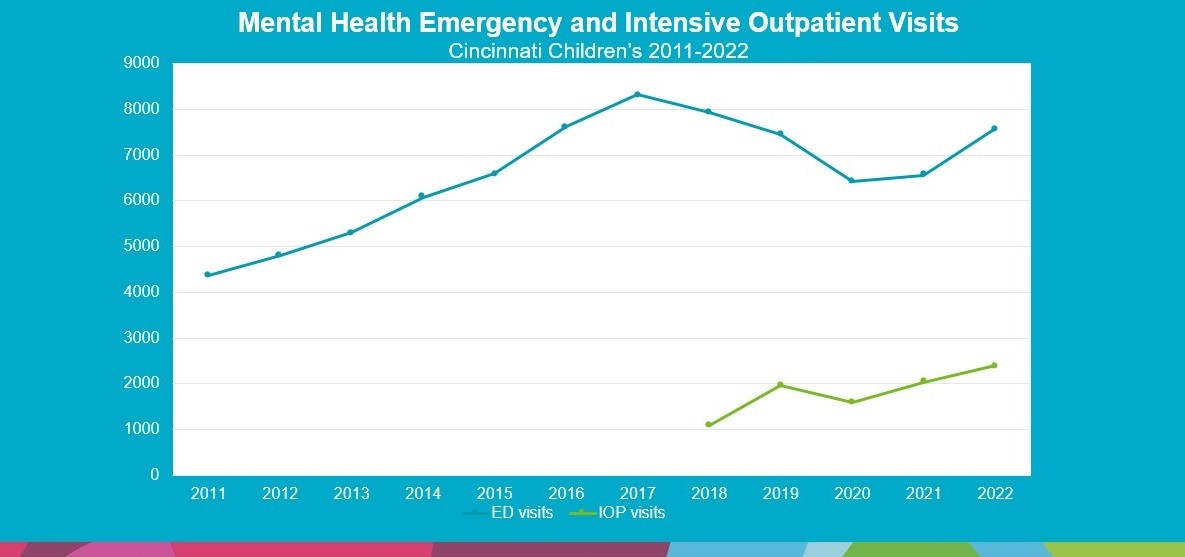
In the Cincinnati region, the number of children seeking emergency care for mental health crises soared 91% from 4,362 visits in 2011 to an all-time high of 8,324 visits in 2017, the study notes.
Recognizing a need to act, Cincinnati Children’s launched a system-wide initiative in 2018 called the Mind Brain Behavior Collaborative to bridge access gaps, integrate mental health expertise into pediatric practices, and commit to long-term research efforts to achieve earlier intervention.
Four Major Changes
The new report describes four pathways the collaborators have followed to transform care, each addressing different levels of the mental health crisis.
The Project ECHO program: This virtual training program was launched to enhance mental health skills for front-line general pediatricians, social workers, school nurses and others working with children in primary care settings. So far, 258 care providers from 153 different practices and organizations have completed courses through Project ECHO.
Embedding psychologists: Beginning with its own hospital-run clinics, Cincinnati Children’s has been supplying more psychologists who work inside pediatric offices, where they can directly help children during a single appointment as well as immediately help connect families to more intensive services when needed. The initiative soon expanded to other community pediatric practices.
So far, this effort has grown from a pilot project involving two psychologists to 12 psychologists working from four hospital-run primary care clinics plus master’s level therapists working under a psychologist’s supervision at 10 community practices.
Rethinking crisis care: Mental health experts at Cincinnati Children’s, much like the rest of the nation, have long wrestled with a gap in services that results in heavy use of emergency departments for crisis care. A significant number of children with new or ongoing mental health conditions can escalate into situations that cannot wait for an advanced-scheduled pediatric visit or therapy appointment. The hospital is serving these children with two programs:
- The hospital’s Bridge clinic diverts patients in crisis, who are not acutely suicidal, from the emergency department to an outpatient clinic set up to provide immediate assessment, intervention, and short-term follow-up.
- Then, instead of a full-blown hospital stay or waiting for weeks or months to schedule follow-up outpatient therapy, many of these children receive care promptly from an Intensive Outpatient Program (IOP). This program provides intervention and monitoring as often as several times a week but allows the child to stay at home.
The paper explores the positive impacts of these efforts. Even though the pandemic drove a surge in emergency mental health visits, Bridge and the IOP helped keep the flow of emergency department visits below the historically high peak that occurred in 2017. (see graph)
Earlier detection: The fourth major initiative, still under development, seeks to sharply improve early detection of mental disorder symptoms to allow much earlier intervention than most children receive now. The medical center has invested more than $10 million in its Mental Health Trajectory program, which seeks to leverage artificial intelligence technology to identify at-risk children early.
This project involves so much complex data that the team at Cincinnati Children’s is working with supercomputers housed at the Oak Ridge National Laboratory in Tennessee to refine their decision support algorithm. Impressively, an early version of the new tool has shown that it can detect signs of clinical-level anxiety in children about 50 days sooner than such children actually receive diagnoses.
A model for others
Experts at Cincinnati Children’s published these findings to provide a roadmap to help other pediatric centers that also are overwhelmed by the mental health crisis.
The paper reports that some of the innovations launched here have become “self-sustaining” because the services could be billed to government and private insurers. Other efforts required charity support.
The co-authors acknowledge that other health systems will have their own resources and challenges. Moving in a better direction will not require following the Cincinnati Children’s approach step-by-step.
“We feel that by describing our journey, we can spark new conversations and novel collaborations across pediatric hospitals,” Cheng says. “We believe specific foundational principles embedded in our system will need to be incorporated into all future successful approaches.”
Meanwhile, building parity in access, quality, and reimbursement between mental and physical health care in an integrated, whole-child approach remains a critical issue to be addressed.
Looking ahead, the co-authors agreed: “Healthcare organizations and payers must place behavioral and mental healthcare needs on equal footing with physical healthcare so that patients and their families receive comprehensive healthcare at every visit.”
| Original title: | Addressing the Pediatric Mental Health Crisis: Moving from a Reactive to a Proactive System of Care |
| Published in: | The Journal of Pediatrics |
| Publish date: | May 13, 2023 |
Research By

My work mainly focuses on the development of a comprehensive system of behavioral healthcare to address the illness and suffering of young people and families struggling with mental illness.

Our lab investigates a number of research questions related to dietary adherence and nutrition in children with chronic and acute health conditions.

As a child advocate, I have promoted the importance of pediatric research including initiation of the “7 Great Achievements in Pediatric Research” campaign (Pediatr Res. 2016;80(3):330-7) and have published on the “Next 7 Great Achievements in Pediatric Research” (Pediatrics. 2017;139(5):e20163803).

An expert in neurology, clinical pharmacology and genomics, Dr. Glauser’s research focuses on clinical pharmacology, pharmacogenetics and antiepileptic clinical trials.

My current focus is on developing clinical interventions and programs to help children and families across the mental health care continuum.

At the Decoding Mental Health Center, we use advanced artificial intelligence (AI) to help those who care for patients with mental health challenges. Our focus is the person, and then the machine. Our mission is to provide clinically useful precision information to families and caregivers.