COVID-19 and Equitable Diffusion of the Vaccines
Post Date: April 20, 2021 | Publish Date:

“Health disparities are differences that should not exist, are modifiable, and that means that we have the opportunity for change.”
Monica Webb Hooper, PhD, National Institute on Minority Health and Health Disparities
During the fifth installment of the Current Topics in COVID-19 Research Seminar Series on April 14, 2021, Monica Webb Hooper, PhD, described the rationale and data supporting concerns about vaccine hesitancy among populations that experience health disparities, existing racial/ethnic differences in common vaccine uptake, and community engaged science that the National Institutes of Health (NIH) plan to support (click here to watch the recording).
Webb Hooper is the Deputy Director of the National Institute on Minority Health and Health Disparities (NIMHD). As an internationally recognized translational behavior scientist and clinical health psychologist, Webb Hooper has dedicated her career to the scientific study of minority health and racial/ethnic disparities, focusing on chronic illness prevention and health behavior change.
RACISM AND HEALTH DISPARITIES
Webb Hooper defined the following terms from a scientific perspective and how each term affects the health of minoritized groups.
Systemic racism and structural racism refer to macro level conditions that limit opportunities, resources, and the well-being of less privileged groups.
“Structural racism has resulted in persistent health disparities, poor health status, and premature mortality, as demonstrated by the current disproportionate burden of morbidity and mortality from COVID-19,” said Webb Hooper.
Institutional racism is described as the systematic distribution of resources, power, and opportunities in our society, to the benefit of people who are white and the exclusion of people of color.
“Within the biomedical research enterprise, structural and institutional racism have resulted in inequitable access to funding, training, and workforce opportunities,” she noted.
Health disparities refer to a specific type of health difference, and the distinguishing factor between health disparities and other forms of differences is that disadvantage is the causative agent (e.g. social, economic, environmental).
The populations who experience health disparities are those who have faced systematically greater obstacles to optimal health and can be characterized in a number of ways, including race, ethnicity, socioeconomic status, gender, sexual orientation, and others.
Considerable racial/ethnic health disparities include shorter life expectancy as well as higher rates of cardiovascular disease, cancer, diabetes, infant mortality, stroke, cognitive impairment, asthma, sexually transmitted infections, dental diseases, and mental illness.
“Health disparities are differences that should not exist, are modifiable, and that means that we have the opportunity for change,” she noted.
Webb Hooper said health disparities existed for centuries before they emerged into a cross-cutting area of scientific study in the 1980s. In 2000, the NIMHD was founded to help advance this area of science and promote meaningful progress and equity. It serves NIH-designated populations with health disparities, including all racial/ethnic minority populations, socioeconomically disadvantaged populations, underserved rural populations, and sexual and gender minority individuals.
RACISM AND SEGREGATION WORSEN HEALTH
Webb Hooper shared that interpersonal racism, resulting from individual level unconscious bias, can lead to receiving inferior medical care among minoritized groups and bias recommendations.
“Robust evidence exists that racial/ethnic minority groups, irrespective of their socioeconomic status, often receive less aggressive medical treatments and are more likely to be denied pain medication, organ transplantation, and are less likely to be offered opportunities to join clinical trials,” she revealed.
Segregation also worsens health, and neighborhoods with primarily racial/ethnic minority residents are also more likely to have lower quality health care and school systems.
“The physical conditions and neighborhood environments that characterize segregated geographic areas commonly make it more difficult for individuals to practice the healthy behaviors that we promote and that we know are health promoting,” she said.
Webb Hooper shared recent CDC data that indicated COVID-19 cases are 1.9 times higher among American Indian or Alaska Native persons, hospitalizations are over three times higher among Hispanic/Latino individuals, and deaths are nearly two times greater among Black or African American individuals.
“We have to get to the root of the problem,” she said. “COVID-19 racial/ethnic disparities are driven by differences in exposure. There’s a structural issue that is taking place here rather than turning to a biological or a genetic one.”
VACCINE HESITANCY AND EQUITABLE DIFFUSION
Webb Hooper shared a recently published NIMHD perspective that pointed to at least two areas that will need close attention: the elevated vaccine hesitancy observed and the need to ensure equitable access to the vaccines.
“I think an important point is that vaccine hesitancy is not uniform within racial/ethnic minority populations,” she said.
The perspective also talks about the complex cognitive and behavioral construct of vaccine hesitancy, which varies by vaccine and is influenced by factors such as complacency, convenience, and confidence. Commonly reported reasons for low vaccine confidence relate to concerns about the speed of development, potential harm from vaccine ingredients, unknown long term health effects, and unanswered questions about whether the vaccine prevents infection and transmission.
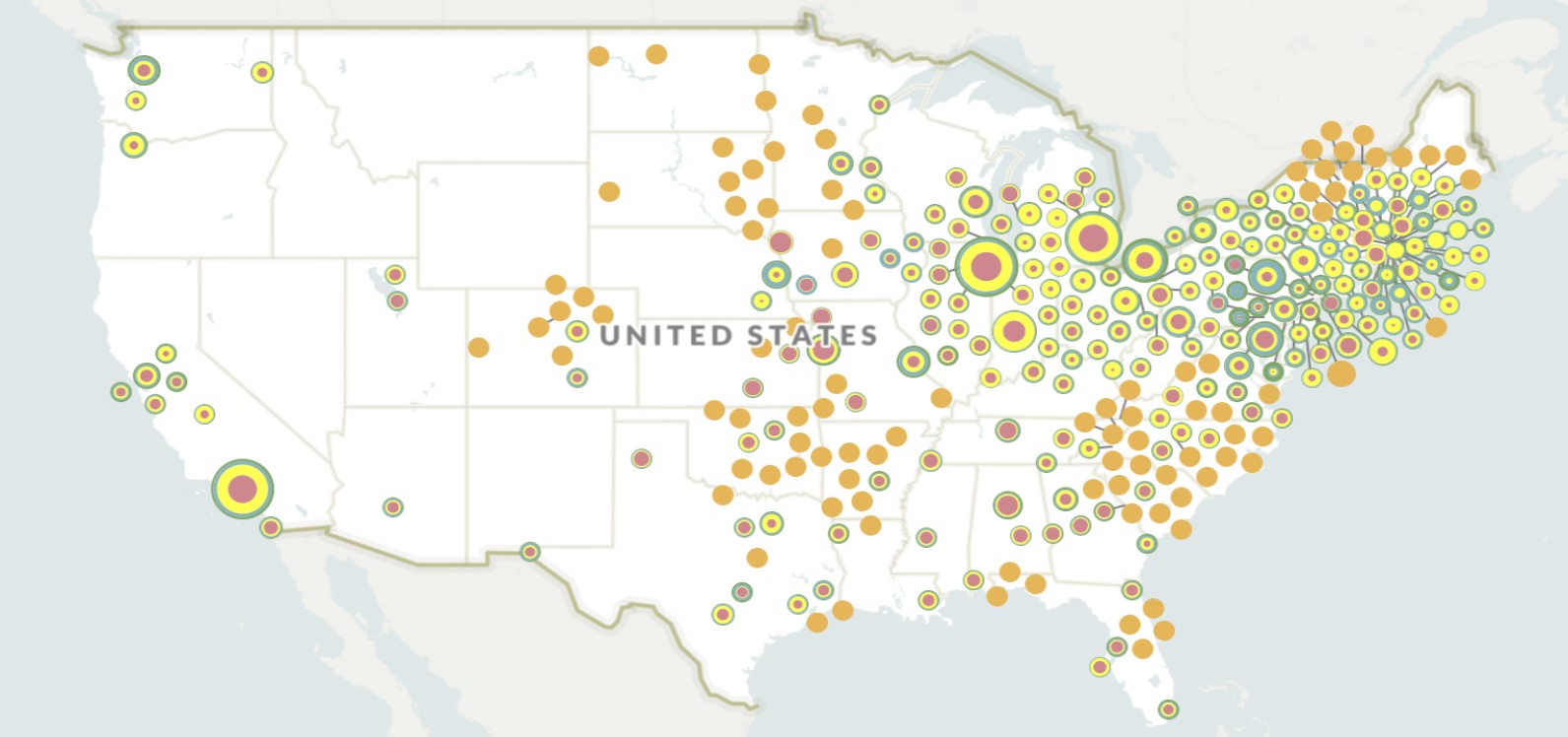
Webb Hooper shared recent data that demonstrate the prevalence of vaccines administered has been increasing for all groups over time, but differences by race/ethnicity may be widening. In addition to vaccine hesitancy, structural factors are also contributors, such as access, digital divide, competition for appointments, misinformation, and distrust.
“There’s an excessive flow of misinformation that makes it hard to separate what is fact from fiction and have confidence in a solution,” she said. “The key concern about this COVID-19 infodemic is that it may have a particularly adverse impact on communities most affected.”
She also shared data from a nationally representative tracking survey called Understanding Coronavirus in America, which not only confirmed that there are racial/ethnic differences in vaccine hesitancy but also that level of education may have a stronger effect on people’s willingness to get the vaccine.
“A college degree is associated with a 43% increase in the likelihood of vaccination intentions,” said Webb Hooper.
REFOCUSING ON COMMUNITY ENGAGED OUTREACH AND RESEARCH
Created this past summer, the NIH’s Community Engagement Alliance (CEAL) Against COVID-19 Disparities has helped to lead outreach and engagement efforts into communities that have been disproportionately affected by the pandemic. CEAL’s overarching goals are to address the COVID-19 misinformation problem, engage trusted voices and community engaged research teams, facilitate the enrollment of underrepresented groups in COVID-19 clinical trials, and invest within the community.
“We move at the speed of trust, and distrust cannot be overcome overnight,” she said. “This is about meeting individuals and communities where they are, being present for the long haul, and importantly, demonstrating trustworthiness.”
The CEAL teams are conducting a variety of activities, such as fostering clinical trial inclusion, conducting community needs assessment and working to respond to those needs, building awareness about how to stay healthy, and providing needed resources such as masks and sanitizer.
“It’s beyond time for us to accelerate meaningful progress, where we’re really seeing interventions that reduce and ultimately eliminate disparities that improve population health and that have a health equity lens,” concluded Webb Hooper.
Watch a recording of the seminar.
RESOURCES AND OPPORTUNITIES
- COVID-19 Vaccine Family Interview (YouTube): featuring Webb Hooper and her parents-in-law who volunteered for a COVID-19 vaccine trial
- UNITE Initiative (NIH): aims to establish an equitable and civil culture within the biomedical research enterprise and reduce barriers to racial equity in the biomedical research workforce
- Research to Address Vaccine Hesitancy, Uptake, and Implementation Among Populations that Experience Health Disparities (NIH)
- Centers for Multiple Chronic Diseases Associated with Health Disparities: Prevention, Treatment, and Management (NIMHD)
- Understanding and Addressing the Impact of Structural Racism and Discrimination on Minority Health and Health Disparities (NIH)
- Inviting Comments and Suggestions to Advance and Strengthen Racial Equity, Diversity, and Inclusion in the Biomedical Research Workforce and Advance Health Disparities and Health Equity Research (NIH)
NEXT UP IN THE CURRENT TOPICS IN COVID-19 RESEARCH SEMINAR SERIES
Natalie E. Dean, PhD, Assistant Professor of Biostatistics at the University of Florida, will present “Evaluating vaccines for emerging infectious diseases.”
As an expert in novel vaccine trial design and analysis, Dean will describe several innovative strategies for evaluating investigational vaccines tailored to the epidemic context.
Join this free virtual seminar at 2 pm (ET) May 12, 2021, via Zoom.