Research Details Reproducible Phenotypes of Pediatric Septic Shock
Research By: Mihir Atreya, MD, MPH
Post Date: July 19, 2024 | Publish Date: July 17, 2024
Multi-center study led by experts at Cincinnati Children’s could lead to new diagnostic tests, targeted treatments, improved outcomes
Few people outside the world of critical care medicine realize that sepsis kills more children every year than cancer does.
In fact, this intense bodily reaction to blood-borne infections kills about 5,000 children a year in the United States and about 3.4 million children worldwide, according to the Sepsis Alliance, an education and advocacy group. Treatment often requires long, intense, and expensive hospital stays. In addition, many children who survive sepsis can face a litany of after-effects.
However, significant variability in the underlying biology among patients experiencing septic shock has long impeded scientific advances in treatment beyond antibiotics and intensive care.
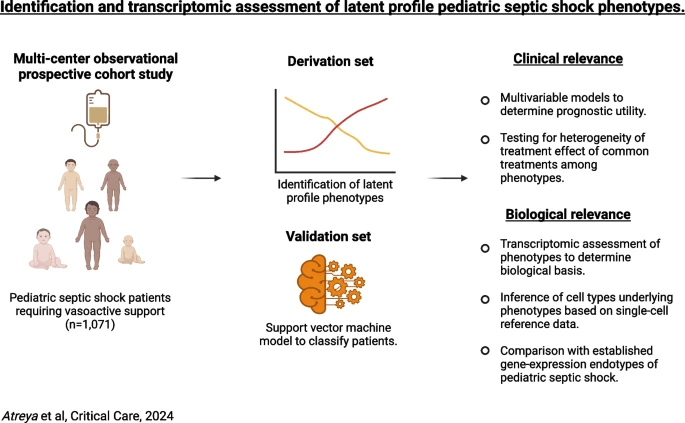
Now, a nation-spanning team of researchers who analyzed more than 1,000 past cases of septic shock, down to cellular changes in gene-expression, report detecting two distinct phenotypes, or signatures, for this dangerous health condition. The findings appeared online July 17, 2024, in the journal Critical Care.
The study was led by Mihir Atreya, MD, MPH, and colleagues in the Division of Critical Care Medicine at Cincinnati Children’s.
“There is a dire need to identify the most at-risk patients and match them with appropriate treatment strategies. However, this has been very challenging to achieve given how rapidly septic shock can develop and evolve,” Atreya says.
Distinct types likely need sharply differing treatments
The study describes patients with “phenotype 1” as facing especially high risk. They appear to have a hyper-inflammatory innate response to the underlying infection, driven by a surge of white blood cells, primarily developing neutrophils. This response can lead to widespread and potentially fatal damage to small blood vessels in multiple organs.

If a rapid gene test can be developed, the research suggests that patients with “phenotype 1” could benefit from special forms of care. These could potentially include maximized precision doses of antibiotics, use of blood purification strategies, or other drugs to modulate the innate immune response system.
However, more research will be needed before changes to critical care practices can be implemented, including cohort studies and clinical trials, the co-authors say.
“While robust sub-classification of patients is a critical first step, we need point-of-care biomarkers to help achieve this at the bedside to inform patient care,” Atreya says.
About the study
This study reflects the latest results from a multi-institutional group of scientists called the Sepsis Genomics Collaborative.
The group’s work builds on a series of discoveries made in recent years by Hector Wong, MD, a leader in critical care medicine research who was serving as vice chair of the Department of Pediatrics at Cincinnati Children’s when he died in 2022. In fact, funds from a National Institutes of Health grant to Wong (NIH R35GM126943) partially funded this study.
Atreya received funding through NIH grants R35GM155165, R21GM151703, R21GM150093 in addition to a Procter K-to-R Scholar Award through the Cincinnati Children’s Research Foundation.
Cincinnati Children’s co-authors on this study included: Andrew Lautz, MD, (IRB lead for the Sepsis Genomics Collaborative), Natalja Stanski,MD, Stephen Standage, MD, Jennifer Kaplan, MD, MS, and Basilia Zingarelli, MD, PhD, all with the Division of Critical Care Medicine.
Co-authors also included researchers with Stanford University, Children’s Hospital of Philadelphia, Nemours Children’s Health, UCSF Benioff Children’s Hospital Oakland, Akron Children’s Hospital, Texas Children’s Hospital, Children’s Hospital of Orange County, Riley Hospital for Children (Indianapolis), Children’s Hospital and Clinics of Minnesota, Penn State Hershey Children’s Hospital, C.S Mott Children’s Hospital (Ann Arbor, MI), University of Florida Health Children’s Hospital, Lucile Packard Children’s Hospital Stanford, Northwestern University, Emory University School of Medicine, Georgia Institute of Technology, and Inflammatix, Inc. (Sunnyvale, CA).
| Original title: | Identification and transcriptomic assessment of latent profile pediatric septic shock phenotypes |
| Published in: | Critical Care |
| Publish date: | July 17, 2024 |








