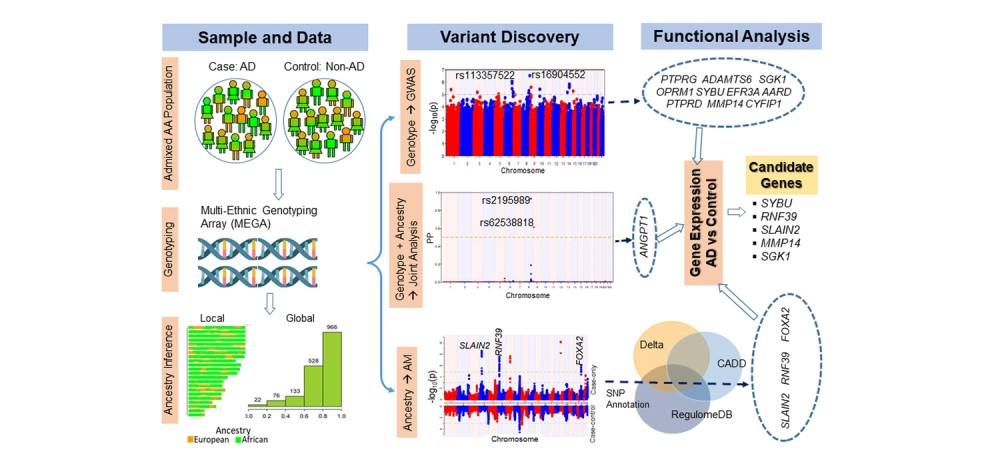
Providing Legal Advocacy Reduces Hospital Admissions by 38%
Research By: Andrew Beck, MD, MPH | Robert Kahn, MD, MPH
Post Date: March 7, 2022 | Publish Date: March 7, 2022

Study in Health Affairs led by Cincinnati Children’s provides rigorous calculation of the impact of medical-legal partnerships, suggests expansion
Ever since pushing a large landlord in Cincinnati to correct toxic housing conditions in 2009, clinicians at Cincinnati Children’s have had powerful anecdotal evidence that a long-running partnership with the Legal Aid Society of Greater Cincinnati was making real improvement in child health outcomes.
Now they have a large body of data to prove it.
In a study published March 7, 2022, in Health Affairs, researchers examined thousands of cases to demonstrate how the Child HeLP program serving southwestern Ohio has resulted in sharp reductions in hospital admissions for children during the year following a referral to the program.
“If this were a pill that demonstrated a 38% reduction across so many kids in terms of hospitalization, every pharmaceutical company in the country would be going after it, and every healthcare payer would be figuring out how to cover it,” says Robert Kahn, MD, MPH, Associate Chair of Community Health at Cincinnati Children’s and the University of Cincinnati, and a co-author of the study.
What is the Child HeLP program?
Launched in 2008, the Child HeLP program (Cincinnati Child Health-Law Partnership) connects pediatric primary care patients and their families to advocates from the Legal Aid Society. Legal aid attorneys rapidly receive referrals and begin providing assistance to lower-income families of children receiving care at the medical center’s primary care clinics.
Overall, the Legal Aid Society helps more than 20,000 people a year. Thousands of referrals have come directly from Cincinnati Children’s since the launch of Child HeLP.
Many cases involve investigating housing conditions when a child winds up needing emergency care for asthma exacerbations. Other common situations include contesting eviction notices that can leave sick children homeless, representing families tangled in public benefits disputes (e.g., unlawful denials or delays of programs like SNAP or WIC), and resolving conflicts with schools when disagreements arise over disability accommodations. Overall, the cases can be as unique as the children involved.
Legal Aid serves seven counties in Southwest Ohio. Child HeLP receives referrals from three Cincinnati Children’s clinics; Avondale, Hopple Street and Fairfield.
Across the country, 450 health organizations have formed medical-legal partnerships, according to the National Center for Medical-Legal Partnership. However, virtually all of the agencies lack the funding to fully meet demand and many areas remain unserved.
“When we started, it was a critical response to an urgent need. We’ve certainly found that we are stronger together. In this kind of partnership, two plus two is absolutely more than four,” says Elaine Fink, JD, Managing Attorney at Legal Aid and a co-author of the study.
Hard-to-measure success
Pinning down the impact of a social program that involves such a wide variety of pediatric health situations was no simple task.
The project involved comparing outcomes for 2,203 children referred to Child HeLP over several years to 100 randomly selected control groups drawn from a pool of 34,235 children who were seen concurrently but not referred. The researchers matched referred with control patients as closely as they could, then applied statistic weighting when some factors could not be matched with precision.
Their methods were closely scrutinized by peer reviewers and editors at the journal. The work also impressed other professionals in the field.
“This is a terrific study,” says Laura Gottlieb, MD, MPH, a professor at the University of California, San Francisco and founding co-director of the Social Interventions Research and Evaluation Network (SIREN), a national research network that studies health care strategies to improve social conditions.
“This work could only be done in a place like a Cincinnati Children’s that has had such a long term dual commitment to addressing families’ social/legal and medical needs and to rigorously evaluating their programs. The study adds substantively to the literature in this area, in this case demonstrating that a strong medical-legal partnership can contribute to decreasing costly and avoidable health care utilization in children.”

Results exceeded co-authors expectations
The study’s corresponding author, Andrew Beck, MD, MPH, Division of General and Community Pediatrics, worked with Kahn, Fink, and others at Cincinnati Children’s and the Legal Aid Society to address the toxic housing case in Avondale. That case started in 2009 with one family facing eviction over installing an air conditioner to help a child with asthma and led to exposing problems—and making improvements—to 19 buildings controlled by the same management group.
As Child HeLP continued to assist families, the team had long sought to evaluate the impact on health outcomes.
“I expected there to be a decrease in hospitalizations because I have seen the legal advocacy of our partners address risks that many of our families face. Even so, I think we found more of a reduction than we expected,” Beck says.
Fink agrees: “I definitely did not assume anything about what this would show. There have been many medical-legal partnerships across the country, and some have been around even longer than ours, but people have not been able to demonstrate the impact through data.”
Next steps
Co-authors say the findings support arguments for expanding the work of medical-legal partnerships.
The Legal Aid Society is seeking a path to receiving funding from health care payers, like Ohio’s Medicaid program, to support more services statewide.
Cincinnati Children’s is expanding the legal partnership concept to families treated at sub-specialty clinics through its new Health Equity Network, which includes teams seeking to eliminate inequities in child health outcomes by race, ethnicity, and socioeconomic status via targeted interventions and best practices.
The hope is that these efforts will result in meaningful, sustainable, and equitable improvements in child health. Increased support from health care payers for such community partnerships, the co-authors say, could accelerate the impact they can have.
Read coverage in the Cincinnati Enquirer

About this study
This work was funded in part by the National Center for Medical-Legal Partnership through a grant from the Robert Wood Johnson Foundation.
| Original title: | Reductions in hospitalizations among children referred to a primary care-based medical-legal partnership |
| Published in: | Health Affairs |
| Publish date: | March 7, 2022 |
Research By