PEDSnet Report Details How COVID-19 Pandemic Has Affected Children
Post Date: November 23, 2020 | Publish Date: Nov. 23, 2020
Analysis of 135,000+ medical records shows the novel coronavirus hits hardest among teens, children with diabetes or cancer, lower-income families, and Black, Latinx and Asian groups
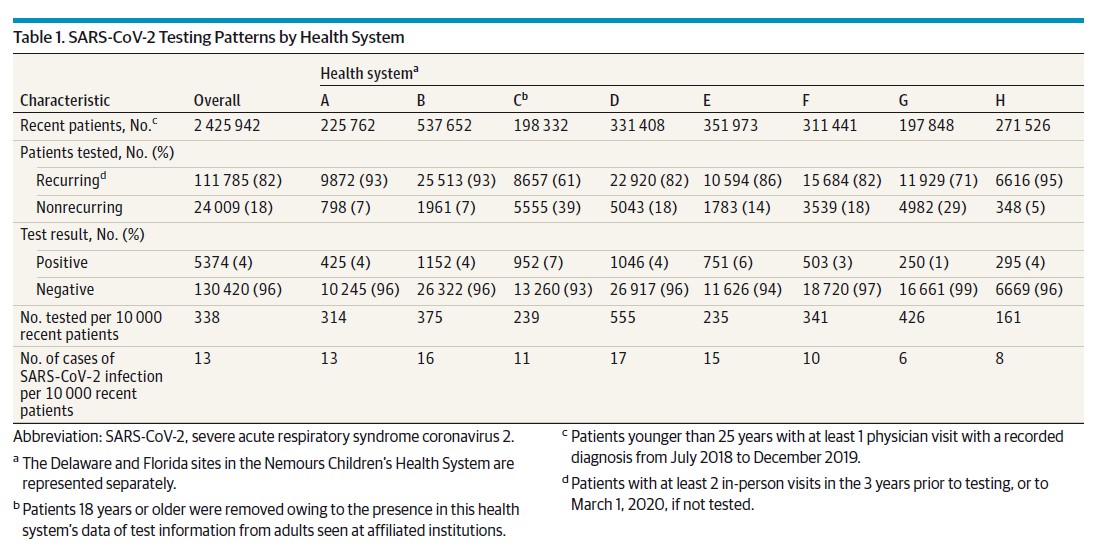
In the most comprehensive analysis to date of U.S. children tested and treated for COVID-19, an organization representing seven of the nation’s largest pediatric medical centers reports that some groups of children are faring significantly worse than children in general during the pandemic.
Findings from the PEDSnet organization—which includes Cincinnati Children’s—were published Nov. 23, 2020, in JAMA Pediatrics. The report is based on electronic medical records data from more than 135,000 children who have been tested for infections from the SARS-CoV-2 virus from Jan. 1 through Sept. 8, 2020.

“These findings are important because they improve our understanding of the impact of COVID-19 in the pediatric population,” says Nathan Pajor, MD, a pulmonary medicine specialist at Cincinnati Children’s and a co-author of the study. “We see that relative to adults, kids are less likely to have severe disease or to die from COVID-19. However, we also notice the disproportionately high rates of infection among Black, Asian and Hispanic children as a clear target of further study.”
PEDSnet centers include Children’s Hospital of Philadelphia; Cincinnati Children’s Hospital Medical Center; Children’s Hospital of Colorado; Nationwide Children’s Hospital; Nemours Children’s Health System; Seattle Children’s Hospital; and, St. Louis Children’s Hospital. Combined, these centers provide care to about 2.5 million children a year.
Highlights of their analysis include:
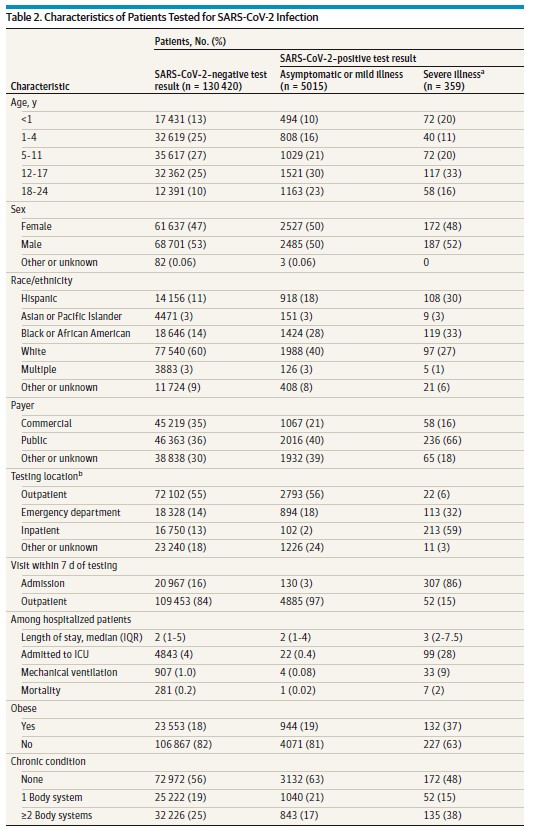
- Like previous, smaller studies, this data shows that children are less likely to test positive and less likely to suffer severe illness when they do get infected.
- Patients of African-American, Hispanic, and Asian race/ethnicity were less likely than white children to be tested. However, they were 2-4 times more likely to test positive.
- Teens and young adults were more likely to test positive than younger children.
- Children covered by Medicaid and other public programs were more likely to test positive than children from privately insured families.
- Underlying cancer, diabetes (types 1 and 2), and other immune-suppressing conditions were indicators of increased risk of severe disease. But children with asthma were not found to be at increased risk of severe illness.
- Among the 5,374 children who tested positive, 7% required hospital admissions. Of those hospitalized, 28% required intensive care and 9% required mechanical ventilation. Of the hospitalized children, eight died. (Case fatality rate: 0.2%)
“Further study is needed to understand the causes behind the variations in positivity rates,” Pajor says. “How much is related to social determinants of risk, such as exposure to air pollution, housing density, or the likelihood of living with a person who must work at an in-person job? How much reflects differences in disease biology?”

Harnessing the Power of Big Data
The PEDSnet data coordinating center is based in Philadelphia, but the concept behind PEDSnet—launched in 2014—was a national cooperative effort among its co-founders, says Tracy Glauser, MD, Associate Director, Cincinnati Children’s Research Foundation.
“Part of the challenge of pediatric research has been that many of our conditions are rare, so that no single institution has enough information by itself to comprehensively tackle certain issues,” Glauser says. “The goal of PEDSnet has been to work out ways for institutions to share data to answer questions we cannot address alone.”
Cincinnati Children’s leaders have invested years of work into launching several data-sharing initiatives, including the Genomics Research and Innovation Network (GRIN) in 2015, becoming the data coordinating center for the Bench to Bassinet (B2B) Program for cardiac research in 2016 and being named the data coordinator for the Rare Diseases Clinical Research Network (RDCRN) in 2019.

Peter Margolis, MD, PhD, chaired the PCORnet Council and serves as the Cincinnati Children’s site principal investigator for PEDSnet. Margolis is Co-Director of the James M. Anderson Center for Health System Excellence and has an extensive track record at building networks for health care quality improvement and research.
“PEDSnet provides a national digital architecture that can harness the power of the electronic health record to advance knowledge,” Margolis says. “Without PEDSnet, gathering the information we are presenting today would have taken years.”
MIS-C Needs Closer Study
While the latest study provides powerful data to address many questions, it also calls attention to the chaotic nature of the early days of the pandemic and how experts dealt with one of the most serious complications affecting children.
Early on children who experienced severe heart-damaging inflammatory reactions were diagnosed with Kawasaki disease, a very rare condition with largely unknown causes. As clinicians noted differences between the new cases and older ones, the diagnosis morphed into Kawasaki-like disease. It has since evolved into “multisystem inflammatory syndrome of childhood” (MIS-C).
The study co-authors say the medical community still has only a partial picture about the impact of MIS-C on children, in part because the rapidly evolving name changes has complicated data gathering. Also, with the pandemic still less than a year old in the U.S., much more study is needed to understand the long-term outcomes of MIS-C.
Much More to Learn
Some of the study’s limitations include not including kids who were infected, or potentially killed, by COVID19 due to lack of testing availability. The study likely undercounts the actual numbers of asymptomatic infected children across the country, and does not address what risk those children may have presented to adults in their lives.
The participating medical centers overcame enormous technical challenges to build this tracking system early in the pandemic. Now, the data can be quickly refreshed to allow further, deeper analysis as the pandemic continues.
“Effective response to SARS-CoV-2 will require rapid but robust development of new clinical and public health practices, based on a better understanding of viral and host biology,” the co-authors say. “This knowledge will be critical not only in caring for severely ill patients, but also in constructing sustainable ways to minimize the disease burden caused by SARS-CoV-2.”
Cincinnati Children’s co-authors on the JAMA study include Janet Zahner, Lead Data Warehouse Analyst.
This work was funded by the Patient-Centered Outcomes Research Institute (RI-CRN-2020-007).
| Original title: | Assessment of 135,794 Pediatric Patients Tested for Severe Acute Respiratory Syndrome Coronavirus 2 Across the United States |
| Published in: | JAMA |
| Publish date: | Nov. 23, 2020 |