Pediatric Cell Atlas Aims to Map the Universe of Cells Responsible for Organ Growth and Disease Prevention
Research By: Peter White, PhD | Bruce Aronow, PhD
Post Date: July 3, 2019 | Publish Date: April 8, 2019
“Constructing normal and parallel disease models for each tissue at the single-cell level provides a tremendous opportunity for translational research”
—Peter White, PhD
Biomedical researchers from 19 centers in Philadelphia, Cincinnati, Boston, San Francisco, Portland, Washington, DC, and other cities have joined with colleagues in five other nations to propose building the world’s first Pediatric Cell Atlas (PCA).
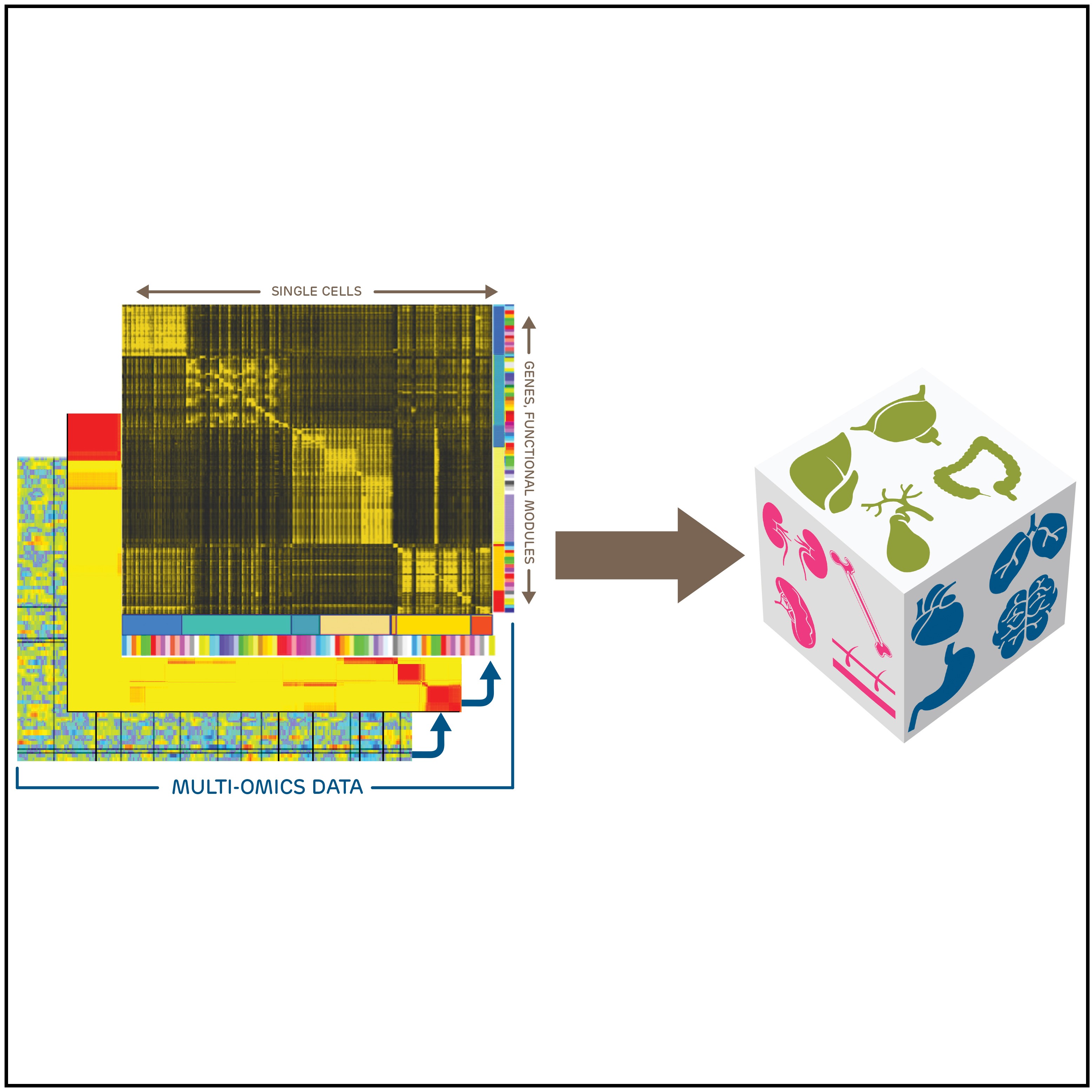
Drawing on recent advances in microfluidics, imaging, computational sciences, and other technologies, a Pediatric Cell Atlas would offer an unprecedented window into the biology of human growth and development. The atlas would detail the compositions, structures and activities of constellations of single cells responsible for the development and growth of all tissues and organs. Building this high-definition view of children’s health will involve bringing together a global coalition of pediatric researchers.
An open-access perspective article laying out the potential value of such an atlas was posted online March 28 in Developmental Cell.
“Part of what’s driving our need to have a deep focus for the Pediatric Cell Atlas is the emerging realization from many ongoing data analyses and studies that healthy organ development is extremely complicated,” says Bruce Aronow, PhD, a biomedical informatics expert at Cincinnati Children’s and a co-first author of the new article. “Each tissue has its own unique context of incredibly specialized, diverse, and extensively communicating cell populations undergoing vastly different gene expression programs.”
The article’s corresponding author is Deanne Taylor, PhD, Director of Bioinformatics at Children’s Hospital of Philadelphia (CHOP). Key contributing authors are Kai Tan, PhD, a scientist with CHOP and the University of Pennsylvania; and Nathan Salomonis, PhD, at Cincinnati Children’s, who co-leads the Cincinnati Pediatric Cell Atlas Program with Aronow.
Another 70 co-authors represent Boston Children’s Hospital, Children’s National Medical Center, Beatrix Children’s Hospital in the Netherlands, the National Institutes of Health, and other institutions.
A GROWTH CHART FOR CELLS
Most parents recall taking their children for check-ups during which a pediatrician logs the child’s height and weight in comparison to national averages. The PCA would compile a vastly more complex collection of growth charts for every type of tissue in the body. This giant new map would help document what is normal for everything from brain development to how the immune system forms. Adding to the complexity, scientists seek to capture how all these maps of normal development shift as a child grows from birth to full adulthood.
Once armed with this set of computational models, scientists could compare similar sets of data from individuals to better understand when and how genetic variations and environmental exposures combine to change the trajectories of development and lead to illness and disease.
“Pediatricians are familiar with the mantra that ‘children are not just small adults,’” says CHOP’s Deanne Taylor. “Children’s diseases, symptoms, outcomes and therapies are often age-dependent, along with differences in physiology, presentation and drug responses compared to those occurring in adults. With this Atlas, we’ll have a standard reference tool showing, at different ages, which cells are doing the work for a child to grow healthily.”
The proposed PCA project addresses what many experts in human development already recognize—a progression of health and disease over a fetal-to-adult continuum. Many lifelong chronic diseases, such as diabetes, asthma and neuropsychiatric conditions, first become apparent during childhood or adolescence. So designing or improving interventions during childhood could yield lifelong benefits, Taylor says. The PCA would provide key evidence for advancing such efforts.
“Constructing normal and parallel disease models for each tissue at the single-cell level provides a tremendous opportunity for translational research,” says senior author Peter White, PhD, Director of Biomedical Informatics at Cincinnati Children’s. “Once these models are in place, they can be tested to see the effect of various interventions, such as drug regimens, genome editing, and tissue re-engineering. This has the promise to significantly speed up the development of novel therapies and further empower precision medicine approaches.”
TECH ADVANCES MAKE ATLAS POSSIBLE
The research community has learned much by extracting genetic data from bulk tissue samples involving thousands or millions of cells. However, not every cell within a section of tissue is always doing the same job, says Salomonis.
“By analyzing data at the single-cell level, much more can be learned about cell types, cell tasks and cell stages,” Salomonis says.
Researchers at Cincinnati Children’s have been working for more than a decade to help set the foundations of a Pediatric Cell Atlas. Advances here include a mouse kidney development atlas built by S. Steven Potter, PhD, in 2008, and work led by Aronow and colleagues to document cell-level developmental details for the brain, heart, lung and gastrointestinal tract.
The technology making this atlas possible, including single-cell RNA sequencing and other advances, has become available only in the past few years.
“Single-cell studies can provide never-before-seen details about how individual organs and tissue grow and function,” Aronow says. “This is expanding our understanding of every part of our body—and particularly so during the dynamic period of childhood growth and maturation. How this process unfolds can shape a child’s health for the rest of their lives.”
DATA TO BE SHARED WORLDWIDE
The pediatric atlas is part of a broader international consortium, the Human Cell Atlas (HCA), which held its initial planning meeting in 2016. Two co-founders of the HCA initiative—Aviv Regev, PhD, of the Broad Institute, and Sarah Teichmann, FMedSci, of the Wellcome Sanger Institute—are co-authors of the current PCA paper.
Atlas data would be shared among project members and with other researchers worldwide. Data would be stored in the HCA’s repository with associated biobanking and data stored in different centers made available to biological researchers.
As the PCA moves forward, it will develop its overall organization, data systems and multiple projects, including pilot studies of specific organs and disease areas.
“The creation of a Pediatric Cell Atlas, as a deep extension within the Human Cell Atlas, will ultimately inform the diagnosis and treatment of pediatric diseases in profound ways that an adult atlas could not,” Aronow says.
| Original title: | The Pediatric Cell Atlas: Defining the Growth Phase of Human Development at Single-Cell Resolution |
| Published in: | Developmental Cell |
| Publish date: | April 8, 2019 |
Research By