Newborn Brains Are Smaller When Exposed to Opioids During Gestation
Research By: Stephanie Merhar, MD, MS
Post Date: April 10, 2025 | Publish Date: April 7, 2025
An important “first dive” into data from the 4-site Outcomes of Babies with Opioid Exposure (OBOE) study features a Cincinnati Children’s expert as co-first author
When pregnant women take opioids during pregnancy, even opioids such as buprenorphine or methadone to treat opioid use disorder, the developing brains of their children can be significantly affected, according to a study published April 7, 2025, in JAMA Pediatrics.
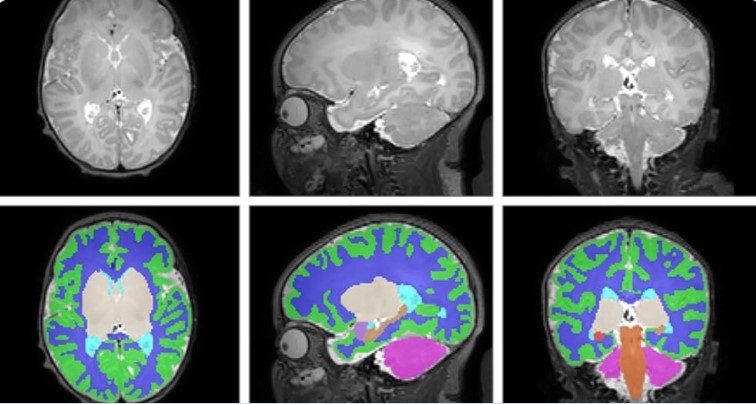
Total brain volume was nearly 5% smaller among 173 newborns with antenatal opioid exposure compared to 96 unexposed newborns, based on magnetic resonance imaging (MRI) scans. More specifically, reduced volumes among opioid-exposed newborns occurred in cortical gray matter, deep gray matter, white matter, cerebellum, brainstem, and the right and left amygdala. There were notable differences in the location and scale of the effects, which varied depending on the type of opioid involved, and whether other drugs were also taken during pregnancy.
“We have known for a while that children exposed to opioids during pregnancy are at risk of later developmental and behavioral problems, but it was hard to know whether that was due to the opioids themselves or other factors such as other exposures or lower birth weight,” says co-first author Stephanie Merhar, MD, MS, a neonatologist at Cincinnati Children’s. “This study was launched because we needed a large study where we were able to control for things like nicotine exposure and birth weight. Our next step is to follow the children in the study to see whether having smaller brain volumes in the newborn period affects later development and behavior.”
The double-threat opioids pose to mothers and children
Nearly 1 in 12 newborns in the United States in 2020 – or about 300,000 infants – were exposed to alcohol, opioids, marijuana or cocaine before they were born, according to the Substance Abuse and Mental Health Services Administration (SAMHSA). Prenatal substance exposure in rural areas often exceeds overall national averages.
Opioids include illegal drugs like heroin and fentanyl, prescription drugs like oxycodone and hydrocodone, and medications for opioid use disorder like buprenorphine and methadone. Opioid use often goes hand in hand with smoking and use of other substances such as alcohol and marijuana. This study compared newborns born to mothers who took opioids only and newborns born to mothers who used other substances as well as opioids. Newborns exposed to opioids plus other substances had smaller brain volumes in more regions compared to those exposed to opioids only.
The most common opioids among participants in the new study were buprenorphine (68.8%) and methadone (26%). Both of these opioids are routinely used to treat opioid use disorder (OUD) and are both recommended for treatment of OUD during pregnancy by the American College of Obstetricians and Gynecologists.
“We know that buprenorphine and methadone are life-saving medications for women with OUD,” Merhar says. “We don’t want to imply that women with OUD should wean off these medications, but we agree with the ACOG recommendation for more research on medically supervised withdrawal in pregnant women.”
The study was praised in an accompanying editorial penned by Nethra Madurai, MD, and Lauren Jantzie, PhD, both of Johns Hopkins University School of Medicine.
Other small studies have shown fetal brain changes caused by opioids. But this multi-center study is the first to be large enough to convincingly distinguish effects linked to opioids versus confounding factors such as maternal smoking, birth weight, education levels.
The study authors “present compelling evidence of the direct effects of opioids on the developing brain,” the editorial states. “Given the prospective design of the trial, they account for other postnatal factors…allowing us to dispel previous uncertainty surrounding the direct impacts of opioids on the brain vs the confounding effects of other environmental factors.”
What’s next?
Having more precise information about the affected parts of the brain could allow scientists to focus on interventions to support healthy brain development for children born after opioid exposure.
“Indeed, we must shift our focus beyond the initial withdrawal symptoms associated with POE [prenatal opioid exposure] if we are to improve the lifelong health and well-being of infants and children impacted by the opioid epidemic,” the editorial states.
Read more about Merhar’s research related to opioid exposure:
- ‘Eat, Sleep, Console’ Approach Slashes ICU Stays for Opioid-Exposed Newborns
- In Utero Opioid Exposure Impacts Fetal Brain Size and Development
- $8M Grant Funds Long-Term Opioid Exposure Study
Don’t Miss a Post:
- Subscribe to the Research Horizons Newsletter
- Follow Cincinnati Children’s Research Foundation on Bluesky: @cincyresearch
| Original title: | Antenatal Opioid Exposure and Global and Regional Brain Volumes in Newborns |
| Published in: | JAMA Pediatrics |
| Publish date: | April 7, 2025 |
Research By

Merhar serves as attending neonatologist at the Perinatal Institute at Cincinnati Children’s. Her research focuses on how the newborn brain can bounce back from insults including brain injury and substance exposure.