Moving Beyond Thoughts and Prayers to Curb Firearm-Related Injuries Among Children
Research By: Meera Kotagal, MD, MPH | Richard Falcone Jr., MD, MPH, MMM
Post Date: January 7, 2025 | Publish Date: Nov. 13, 2024
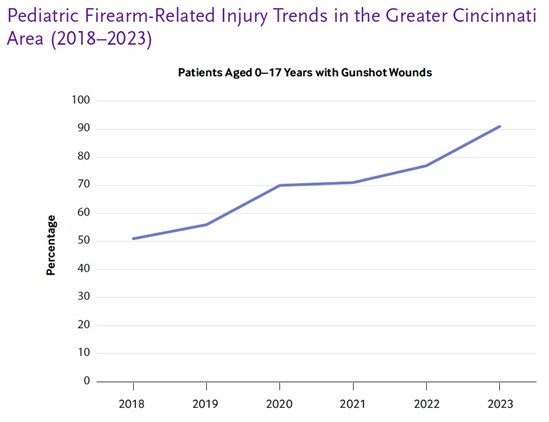
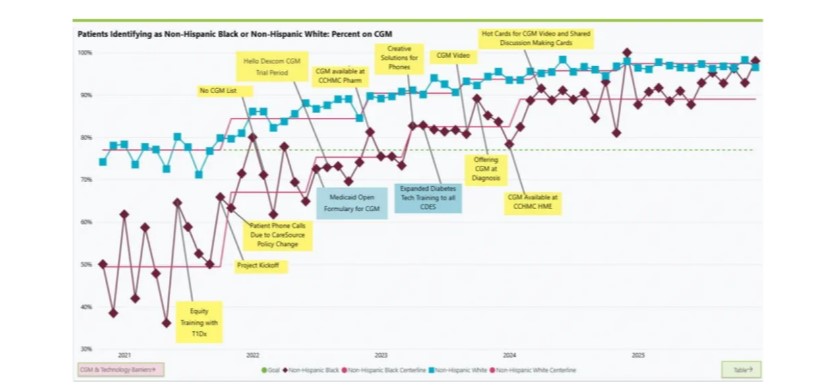
Firearm-related injuries are the leading cause of death for children in the United States. This epidemic has increased dramatically in the last several years, and impacts countless children, families and communities—with higher rates of injuries among disadvantaged communities.
Experts at Cincinnati Children’s explain in a commentary published in NEJM Catalyst in December 2024 that reducing this deadly toll requires deep commitment, practical strategies, and robust, well-supported teams focused on evidence-based approaches to change.
Cincinnati Children’s Meera Kotagal, MD, MPH, director of Trauma Services; Robert Kahn, MD, MPH, vice president of Health Equity Strategy; Victor Garcia, MD, founding director of Trauma Services; and Richard Falcone, MD, MPH, MMM, Chief of Staff, penned the commentary stressing the need for academic medical centers to address this critical public health crisis. This team is leading by example through the Firearm-Related Injury Task Force at Cincinnati Children’s. They detail the necessary elements for it to be a success in the paper.
One of the commentary’s defining arguments is the difficulty institutions can have applying their resources to such a formidable task.
“Reducing this toll [of firearm-related injuries] will require addressing underlying problems that are dauntingly complex, deeply engrained in structural racism and intertwined with a volatile political environment surrounding the rights of firearm owners,” the piece says.
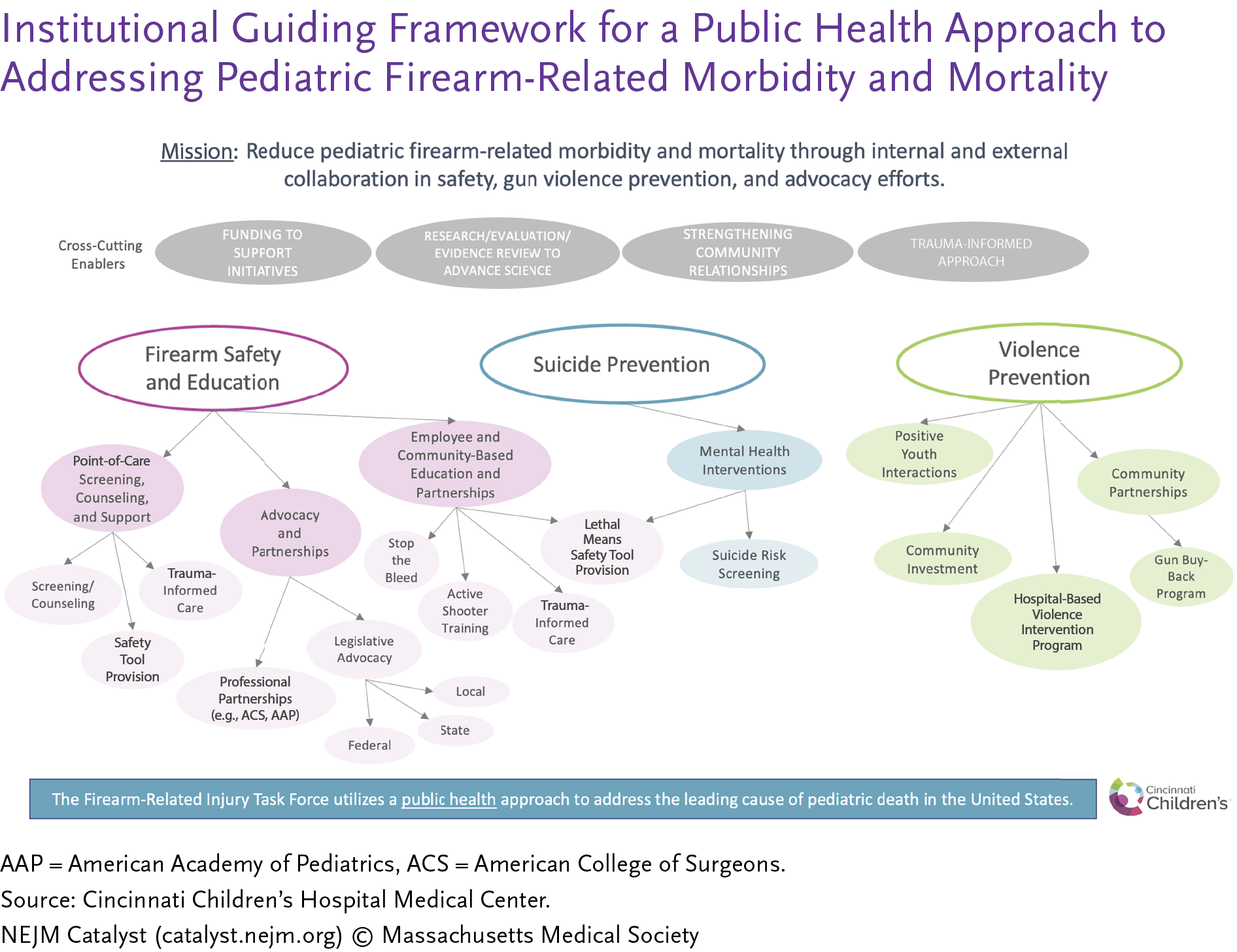
The commentary outlines steps the team took in establishing the task force and ensuring its sustainability and impact. The first step was to gather a multidisciplinary team from across the health system who either were actively involved in efforts to address firearm-related injuries or held key positions vital to tackling the complex problem. Next, they built out a framework for the task force in which three guiding themes or pillars emerged: firearm safety and education, suicide prevention, and violence prevention. With this in mind, they created key steps to help coordinate existing efforts within the health system and promote synergy among them:
- Identify leaders who care for patients with firearm-related injuries or have related clinical or research interests.
- Convene these leaders to develop an understanding of ongoing efforts across the organization that could be brought together with synergy and catalyzed by the task force.
- Identify a clear mission and scope for the task force.
- Create a structure with tangible next steps, measurable outcomes and a process for maintaining the momentum of the task force’s work.
- Develop a communication strategy to describe the efforts both internally and externally.
While these initiatives are still being implemented, the task force has developed key metrics for measurement and tracking on a dashboard that will eventually demonstrate their impact on reducing firearm injuries:
- Number of children (0–18 years of age) sustaining firearm-related injuries.
- Number of employees trained in firearm screening and counseling.
- Number of employees completing Stop the Bleed and Active Assailant training.
- Number of patients with firearm-related injuries enrolled in nascent hospital-based violence intervention programs.
Looking to the future, the team has obtained a $600,000 grant from the City of Cincinnati to build the first joint pediatric and adult hospital-based violence intervention program together with UC Health. Additionally, the team has worked to procure bleeding control kits for the health system, and the development of a mandatory Stop the Bleed and Active Assailant education module for 19,000 Cincinnati Children’s employees.
The team is further collaborating with the City of Cincinnati to help devise a city-wide strategy for gun violence reduction, including a focus on action teams to test and implement interventions, building off root causes identified by community members through multiple focus groups and listening sessions.
The team also is leveraging the task force’s framework in collaboration with the American College of Surgeons Committee on Trauma to create a website with resources for trauma centers across the country.

Meanwhile, Joe Real, MD, MEd, and Matt Zackoff, MD, MEd, have launched the Firearm Safety Counseling Virtual Reality Program at Cincinnati Children’s to give clinicians a safe, realistic setting to practice having conversations about firearm safety and secure storage with patients and families. Now they are embarking on a multisite partnership to spread their innovative program across the country.
Don’t Miss a Post:
- Subscribe to the Research Horizons Newsletter
- Follow Cincinnati Children’s Research Foundation on Blue Sky: @cincyresearch.bsky.social
| Original title: | Moving Beyond Thoughts and Prayers: Creating a Firearm-Related Injury Task Force |
| Published in: | NEJM Catalyst |
| Publish date: | Nov. 13, 2024 |
Research By

As a pediatric surgeon, I specialize in trauma, surgical oncology (including renal tumors and neuroblastoma) and colorectal surgery. As part of my global surgery focus, I also work in Uganda, in partnership with Ugandan pediatric surgeons, to help strengthen the health care system’s ability to care for children with surgical diseases.

I treat children from birth to adolescence who need general and thoracic surgery and emergency care.