Is Now the Time for Circadian Medicine?
Research By: John Hogenesch, PhD | Marc Ruben, PhD | Gang Wu, PhD
Post Date: July 1, 2019 | Publish Date: Sept. 12, 2018
“It doesn’t matter if you’re male, female, young or old, or what your ethnicity is, your body’s internal clock regulates half your genome.”
—John Hogenesch, PhD
The precise time you take your medicine could make all the difference in its effectiveness, say researchers here.
John Hogenesch, PhD, Director, Center for Chronobiology at Cincinnati Children’s, led a team of several collaborators on two recent studies that significantly advance the science of circadian medicine. The work involved collaborators from several divisions at Cincinnati Children’s, as well as experts at Vanderbilt, the University of Pennsylvania and Procter & Gamble.
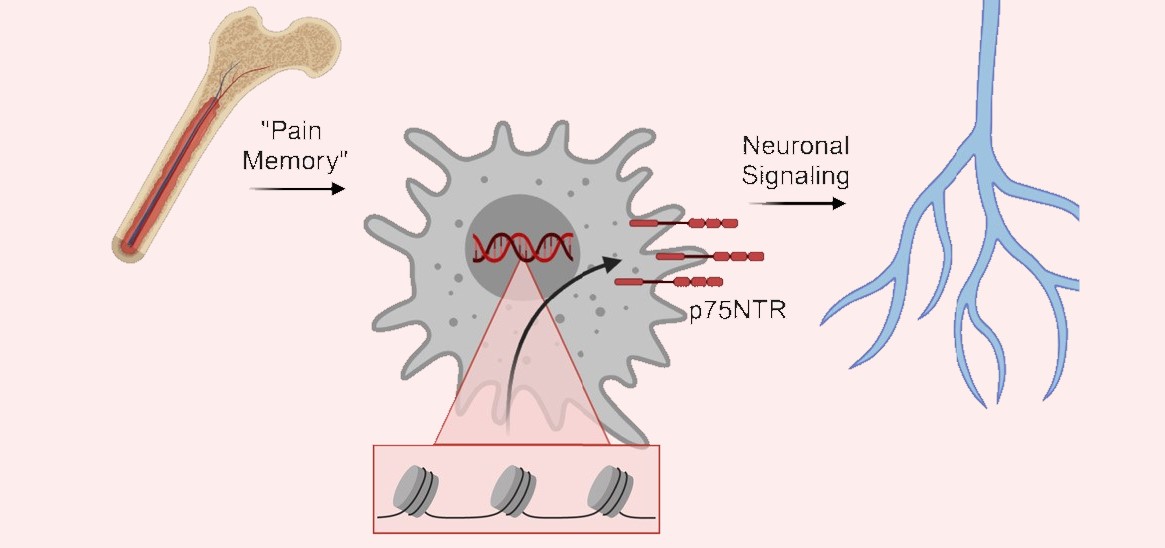
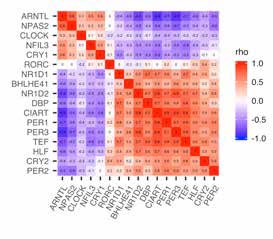
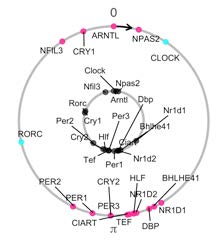
Marc Ruben, PhD, was first author for findings published Sept. 12, 2018, in Science Translational Medicine, that found a surprising number of genes affected by circadian rhythms. The team developed the CYCLOPS algorithm (CYCLic Ordering by Periodic Structure) to analyze thousands of human tissue samples to measure the timing of gene-to-tissue interactions in 13 tissue types.
Our bodies have many clocks
“We identified rhythms in gene expression across the body in a large and diverse group of people,” Hogenesch says. “It doesn’t matter if you’re male, female, young or old, or what your ethnicity is, your body’s internal clock regulates half your genome.”
Says Ruben, “Overall this connects thousands of different drugs, both approved and experimental, to nearly 1,000 cycling genes.” Many of these genes code for proteins that help transport or metabolize drugs are themselves drug targets—including genes with well-known connections to the cardiovascular system.
The ultimate ‘wearable’?
Next, first author Gang Wu, PhD, and colleagues published findings Oct. 30, 2018, in PNAS, concluding that a number of cycling genes in the skin function are more effective biomarkers for measuring an individual’s particular internal clock than current methods based on genes found in the blood. This study included NIH funding and other sources. Critical data was provided by Procter & Gamble, which also paid for the clinical work involved.
“We showed that human epidermis has a stronger clock than blood and developed a panel of biomarkers that can phase individuals to within three hours from a single sample,” the authors wrote.
The researchers emphasize that additional studies are needed before the findings can be applied to clinical practice. But the findings suggest that a practical method may soon become available to allow doctors to instruct patients more precisely on when to take medications at peak times for maximum effectiveness, or at trough times to minimize side effect risks.
Listen to BBC interview with Dr. Hogenesch
Learn more about the chronobiology research happening at Cincinnati Children’s
| Original title: | A database of tissue-specific rhythmically expressed human genes has potential applications in circadian medicine |
| Published in: | Science Translational Medicine |
| Publish date: | Sept. 12, 2018 |
Research By