Introducing CuSTOM: our Center for Stem Cell and Organoid Medicine
Post Date: June 30, 2019 | Publish Date: Winter 2018
Eight years ago, Cincinnati Children’s scientists first used pluripotent stem cells to mimic natural human development and grow working human intestine in a lab. Today medical center doctors can bioengineer the gastrointestinal tissues of sick children to find clues about a child’s disease and how to treat it.
Building on this early research advancement in personalized medicine, Cincinnati Children’s recently launched the Center for Stem Cell and Organoid Medicine (CuSTOM). The center will accelerate the transfer of stem cell-organoid technology from the research lab to practical clinical tool.
Organoid technology has the potential to solve several current medical and research challenges, according to Aaron Zorn, PhD, the new center’s Director. The technology can address a shortage of organs available for transplant. It can eliminate the lack of human modeling systems for developing drugs and testing their safety and effectiveness before going into expensive clinical trials. The technology also gives researchers a first-in-class physiological platform to conduct laboratory research on living diseased tissue, which cannot be done on patients.

Organized to Collaborate
The new center is organized as a highly collaborative, multi-disciplinary center of excellence that integrates scientists, clinicians, geneticists, surgeons, bioengineers and entrepreneurs. It is believed to be the first dedicated facility at a pediatric medical center focused on advancing pluripotent stem cell-organoid technology and translating its potential to clinical practice.
“We have this convergence of transformative breakthroughs in organ-generation technology at Cincinnati Children’s, and it’s critical that we speed up the translation cycle so patients can benefit more quickly. This is, by definition, personalized medicine,” Zorn says.
Built on Science
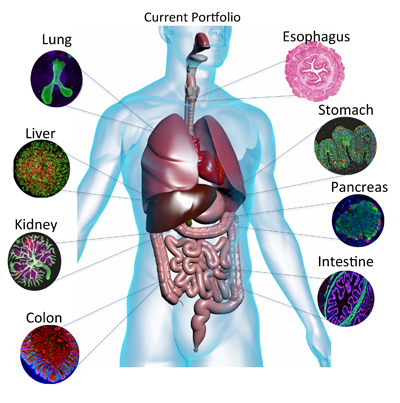
In a series of studies published since 2010, medical center researchers led by developmental biologist James Wells, PhD, the new center’s Chief Scientific Officer, used human pluripotent stem cells to bioengineer gastrointestinal tract tissues that mimic natural human development in a laboratory. Scientists tissue-engineered the small intestine, colon, stomach, and human intestine with functioning enteric nerves and then used these to study different gastrointestinal diseases.
Medical center researchers also bioengineered mini livers in landmark studies led by Takanori Takebe, MD, the center’s Associate Director of Commercialization. Liver organoids hold the nearest-term clinical potential as a personalized platform to test the toxicity or efficacy of existing and new drugs in organoids grown from patients’ cells for diseases such as drug-induced liver injury and steatohepatitis.
The lab-bioengineered tissues reveal the precise genetic and biological processes that cause disease, say researchers. Mini organs can identify the unique biological characteristics of a disease in a single person.
The overall effort to study potential applications for organoid technology is led by Michael Helmrath MD, MS, Division of Pediatric General and Thoracic Surgery, the new center’s Associate Director for Translational Research .





