Hybrid OR Blazes Path Forward for Pediatric Surgery and Interventional Radiology
Post Date: February 14, 2021 | Publish Date:



Cincinnati Children’s marks 3rd anniversary of innovative space for complex procedures
For the family of Leena Shamsi and the surgeons and interventional radiologists at Cincinnati Children’s, Valentine’s Day 2018 was a day to remember.
On that day, a team of clinicians completed a set of procedures that allowed the 5-year-old girl to return to walking, running and playing like 5-year-old girls should. In the process, they began to demonstrate the potential of the next evolution in pediatric surgical technology—the hybrid OR.
“By that time, Leena had been in the hospital for more than three months. When she needed another surgery almost a year later, she did not want to go back to the hospital. The fact that they could combine procedures so that she only had to go in once instead of at least twice was a huge relief,” says Leena’s mom, Umara Raza.
While Leena, now 8 years old, is growing up closer to her relatives in Houston, the leaders who launched one of the first hybrid ORs to be established in a pediatric medical center are looking back on three years of progress that has included more than 1,600 procedures. After starting with complex vascular interventions that helped patients such as Leena, the Phillips Azurion Hybrid OR at Cincinnati Children’s has demonstrated surgical advances in pulmonology, gastroenterology, airway reconstruction, neurosurgery, and more.
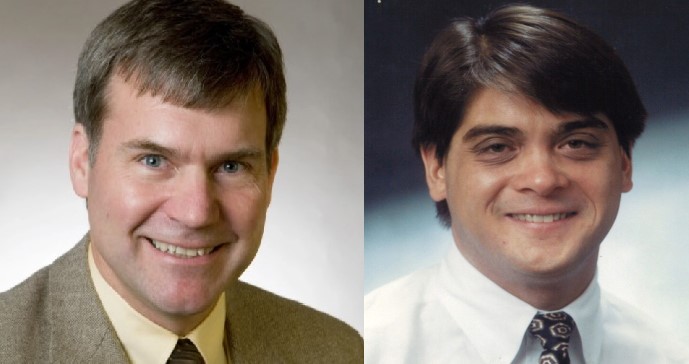
“This new modality is not just about having a combination of radiological and surgical equipment in one room. It’s the realization of a philosophical approach of bringing people together from various areas of expertise to help do the best thing for the patient,” says Daniel von Allmen, MD, Surgeon-in-Chief at Cincinnati Children’s.
In some medical centers, departments of radiology and surgery have waged fierce turf battles over who controls the ongoing evolution of image-guided surgery. At Cincinnati Children’s a culture of collaboration enabled a marriage that transformed a concept for better outcomes into a reality for families.
“In adult medicine, hybrid ORs have traditionally been standalone projects for one subspecialty, such as cardiovascular surgery,” says John Racadio, MD, Director of Interventional Radiology Research and Innovation at Cincinnati Children’s. “But the downside of limiting this approach to just one subspecialty is that an amazing technology winds up not getting used more broadly. Taking a wider view is what we’ve been trying to do from the very beginning here.”
Embracing Evolving Technology
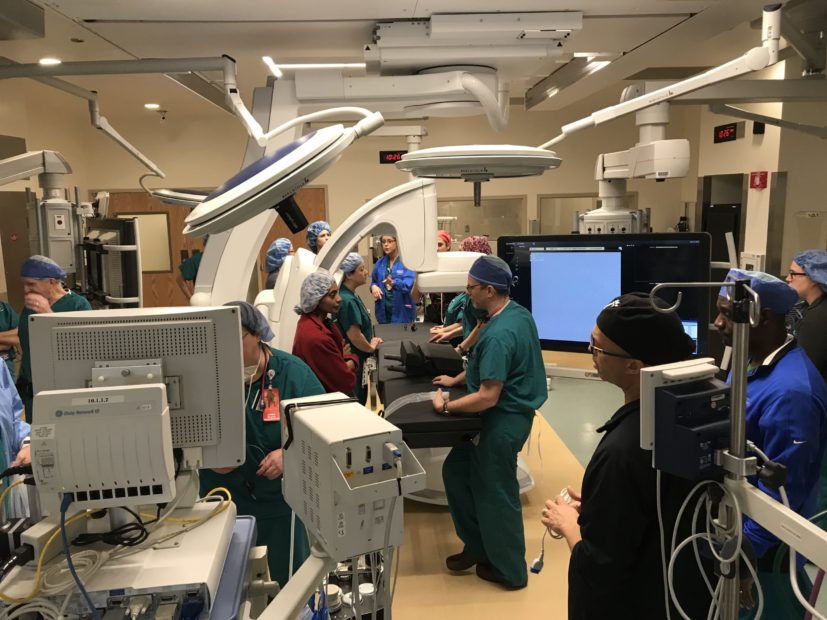
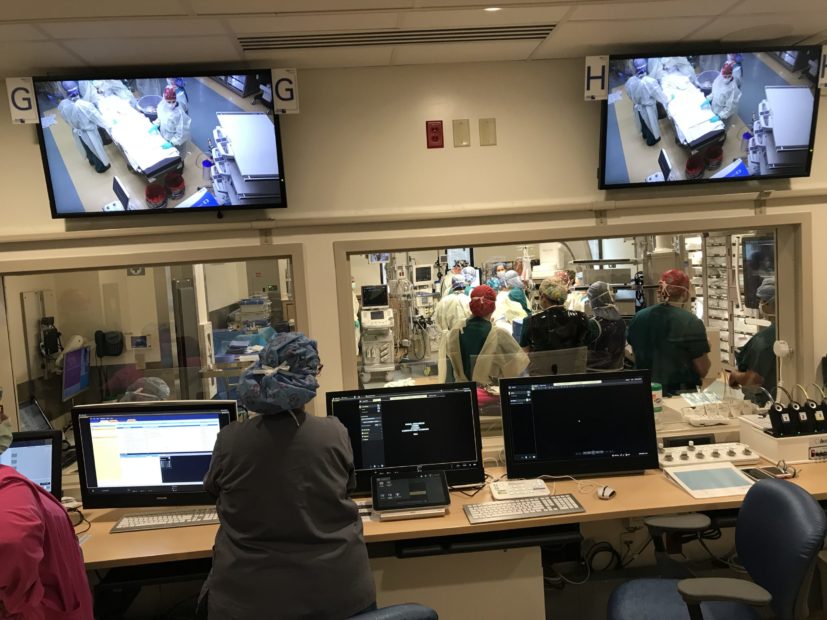
The Hybrid OR is equipped with a range of tools to support image-guided and minimally invasive procedures all within a space roomy enough to accommodate large teams of professionals for especially complex cases. Technologies include fluoroscopy, ultrasound, and Cone Beam computerized tomography to guide procedures.
For adult hospitals, hybrid ORs have become well-established, especially for common cardiovascular procedures. However, applying the concept to pediatric surgery required a unique approach capable of serving teams focused on the brain, heart, airway, digestive system and more.
“Unlike adult care, pediatric surgery rarely involves large numbers of any particular procedure. While the advantages of a hybrid OR include speed and efficiency, we understood from the beginning that a pediatric hybrid OR also needed maximum flexibility,” von Allmen says. “We believe we have achieved that balance.”

Faster AND more precise
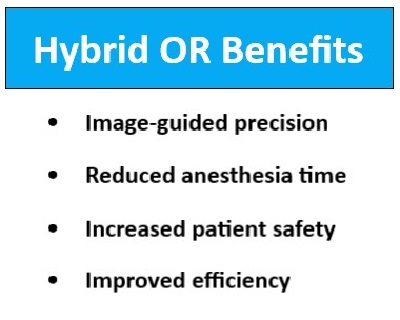
Surgeons at Cincinnati Children’s say the hybrid OR enables a variety of cases that either could not be done as a single operation, or would require extended anesthesia time to allow moving patients between separate imaging and surgical suites.
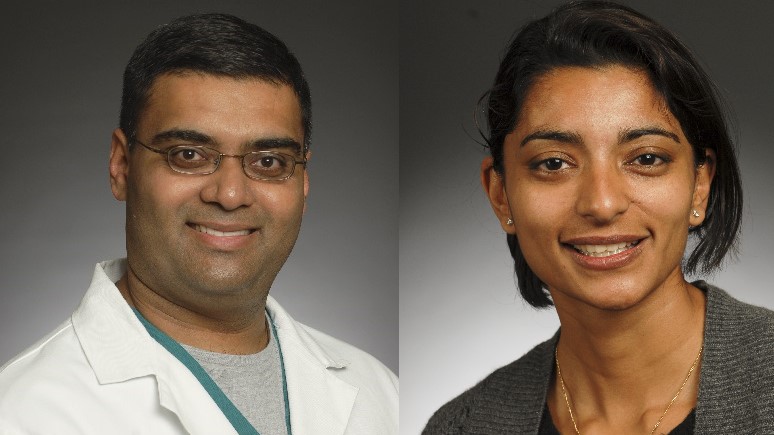
Interventional radiologist Manish Patel, DO, and Roshni Dasgupta, MD, MPH, Surgical Director, Vascular Malformations Clinic, led a team of experts who helped rescue Leena’s leg.
Leena was born with several health complications, including severe hearing loss that led to a cochlear implant at age 14 months and a vascular malformation in her right leg that became a more severe problem as she grew.
Doctors first noted the possible vascular issue while examining Leena in the months after her implant procedure. The family had noticed that Leena’s foot had begun to swell for no obvious reason. Initially the potential malformation seemed minor and unnecessary to treat at the time.
Then, when Leena was almost 5 years old, she came down with influenza and strep infections. The resulting inflammation combined with the vascular malformation disrupting blood flow sent Leena into sepsis. Doctors found damage from her foot up to her knee.
“She was severely ill. She almost died,” says her mother Umara. “She was in the hospital for about three months and had several procedures on her leg.”
That series of treatments saved Leena’s life, but more work was needed to further repair her leg.
A year later, the team at Cincinnati Children’s proposed using the new hybrid OR to do the work.
Rather than conducting one interventional radiology procedure called a venogram to map the location of the vascular malformation and a corrective surgical procedure later, the hybrid OR allowed the entire process to be completed during one operation.
Beyond being a relief for a child tired of hospital encounters, doctors say the hybrid OR approach reduced the time Leena spent under anesthesia and avoided risks that can occur when patients must be moved between radiology and surgical suites.
Digital ‘eyes’ for delicate procedures
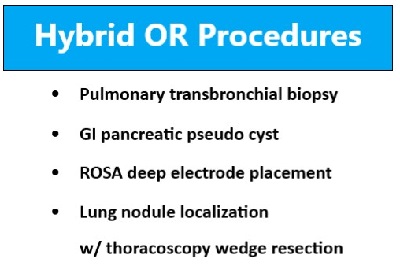
Using a hybrid OR is not required for every child facing a surgical procedure, von Allmen says. But there are clear benefits for several types of procedures, including guiding instruments to reach precise locations within the lungs, planning and performing complex airway reconstructions, even placing electrodes deep inside the brain.
In one recent case performed by experts in the Aerodigestive and Esophageal Center at Cincinnati Children’s, the hybrid OR accommodated 22 physicians and staff from pulmonary medicine, otolaryngology, gastroenterology and other divisions who were involved in the patient’s care, von Allmen says.
“This was a child who had been treated at another hospital for a long time and was sent here as a last resort. We used that large group to plan a very successful procedure, which was performed at a subsequent time,” von Allmen says. “Now the child is back home, growing up in New York.”
Pediatric interventional pulmonologists have long been hesitant to attempt to collect biopsy samples in certain locations in the lung, Racadio says. With so many branching pathways and limited guidance capability from conventional live x-ray devices, clinicians could not feel confident that the samples they collected were in fact from the targeted area.
However in the hybrid OR, pulmonologists and interventional radiologists can use a combination of cone beam CT scanning and 3D software to create real-time maps of complex bronchial pathways leading to a 3D volume rendering of the lung abnormality. Live fluoroscopy can then be superimposed to help navigate the bronchoscope precisely to the target for trans-bronchial biopsy. In an important recent case, the care team was concerned that cancer might have returned for an 8-year-old child previously treated for lymphoma. A PET scan had detected a blockage deep within the child’s lungs that appeared to require a potentially dangerous biopsy.
However, while using an ultrasound-tipped probe in the hybrid OR and from intra-operative cone beam CT imaging, the team determined that the blockage was less severe than it initially appeared. Instead of a tissue-damaging biopsy, the team performed a safer, pathway-clearing lavage procedure. The collected fluids turned out to be mucus rather than a tumor.
“While endobronchial ultrasound has been performed for adults with lung cancer, it has rarely been attempted in children. We think that the combination of intra-operative cone beam CT navigation and endobronchial ultrasound, as in this case, will open new frontiers for pediatric trans-bronchial intervention,” Racadio says.
In another complex case, the hybrid OR proved useful in a sophisticated epilepsy procedure called ROSA deep electrode placement. These operations can last for hours, in part because the patient begins in the surgical suite for initial electrode placement, then must be moved to a radiology suite to confirm that the locations were correct, and then moved back to the surgical suite if adjustments are needed.
In the hybrid OR, the entire process happens in one room.
“A year ago, we never would have thought we would be doing epilepsy procedures in the hybrid OR,” von Allmen says. “But (Francesco Mangano, DO, Director of Pediatric Neurosurgery) and his team saw the potential and worked with the manufacturer to achieve the imaging quality they needed.”
Unique research opportunities
Unlike nearly any other pediatric center, Cincinnati Children’s actually has two hybrid ORs—one for children, and a second one for research. In fact, the Cincinnati Children’s Interventional Radiology Translational Research and Simulation Lab began testing and practicing with the technologies of the hybrid OR using phantoms and animal models several years before procedures were performed on children, von Allmen and Racadio say.
As teams learn from these procedures, collaborators are sharing their findings—including hosting the first Imaged-Guided Pediatric Surgery Consortium meeting held November 2019.
Racadio, von Allmen and colleagues co-authored a review article about hybrid ORs for pediatric surgery in March 2018 in Current Surgery Reports. In April 2018, team members also presented cases at meetings of the American Pediatric Surgical Association and the International Pediatric Endosurgery Group.
In August 2019, von Allmen and Racadio also discussed the collaboration on the podcast “This Week On The BackTable.”
What’s next?
In the research lab, orthopedic teams are studying how to best use hybrid OR technology for spine surgeries that require precise screw placement. Another project is exploring the use of virtual reality goggles that can allow surgeons to see projected digital guidance images without depending as much on monitors across the room.
“We’ve already seen the hybrid OR change the way we perform a number of procedures,” Racadio says. “As we continue working, we will see even more innovative applications in the years ahead.”







