Hospitals, Clinics, Schools Team Up to Improve Asthma Outcomes
Research By: Carolyn Kercsmar, MD | Mona Mansour, MD, MS | Andrew Beck, MD, MPH
Post Date: July 3, 2019 | Publish Date: Nov. 1, 2017

“Beyond the statistics, what we’re really doing is reducing the disruption that families face when their children get hospitalized or come to the emergency room for asthma exacerbations.”
—Carolyn Kercsmar, MD

An ambitious community-wide asthma care improvement project demonstrates that, yes, the needle can be moved.
Hospitals and clinics across America battle daily to help low-income children with asthma successfully manage their condition. Yet a litany of challenges drives higher rates of return visits: lack of money for medications, lack of transportation, instability in the home, increased risks from pollution and poor housing conditions, and more.
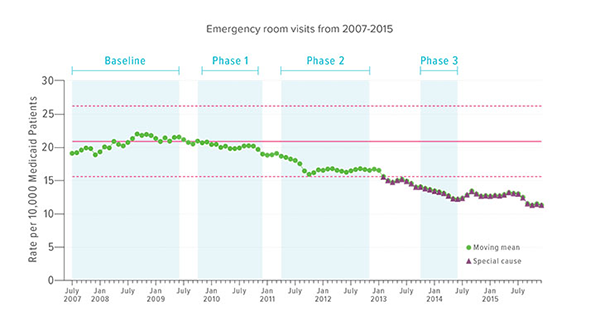
But a five-year project organized by Cincinnati Children’s and a group of committed community organizations demonstrated that outcomes can be improved. In fact, the collaborators managed to slash hospital return visits within 30 days of discharge among Medicaid-insured children by 41 percent.
The study was led by Carolyn Kercsmar, MD, Director of the Asthma Center; Mona Mansour, MD, MS, Director of Primary Care; and Andrew Beck, MD, MPH, who is based in the divisions of General and Community Pediatrics and Hospital Medicine. The project involved forming a large learning network of people working in hospital and outpatient care settings who collaborated with families, pharmacies, school nurses and city health officials.
“I do think this study is fairly unique in the number of partners we brought together, the scope of the work, and the ability to impact outcomes,” Mansour says.
“One of the hardest metrics to move in asthma care is high utilization of emergency services,” Kercsmar says. “But beyond the statistics, what we’re really doing is reducing the disruption that families face when their children get hospitalized or come to the emergency room for asthma exacerbations.”
A 3-phased approach
The scale of the asthma challenge here is daunting. In Hamilton County, the home location of Cincinnati Children’s, more than 36,000 children have asthma, including more than 13,000 covered by Medicaid. Nearly all the hospital care for those children is provided by Cincinnati Children’s.
The medical center launched its Asthma Improvement Collaborative in 2007, with improvement efforts kicking off in 2009.
A three-phased set of improvements flowed from these efforts. The first focused on hospital-based changes, the next on outpatient care, and the third on a wider set of community goals.
Overall, the project reduced asthma-related hospitalizations from 8.1 to 4.7 per 10,000 Medicaid patients per month. Asthma-related emergency visits fell from 21.5 to 12.4 per month.
“This approach is now baked into how we do our work,” Mansour says.
INPATIENT FOCUS ON MEDS-IN-HAND
The network quickly determined that vital asthma medications prescribed after hospitalization often went unfilled at local pharmacies. In response, the hospital began sending families home with a full month’s supply.
By 2010, more than 90 percent of asthma patients went home with a 30-day supply of inhaled controller medications, up from just 50 percent in 2008.
OUTPATIENT FOCUS ON ACTION PLANS, TARGETED DELIVERY
Phase Two improvements focused on baseline asthma control among children served by the medical center’s primary care clinics. Teams implemented a bundle of best practices that included consistent collection of testing data, creating asthma action plans, and enrolling the highest-risk families in care coordination programs.
Two challenges surfaced. Some families needed more asthma management training. Others faced ongoing trouble picking up medications. This led to working with a local pharmacy to launch a targeted delivery service.
By the end of June 2015, the effort enrolled 763 patients into care coordination programs. Of those, 394 “graduated” with demonstrated improved understanding of asthma management. Another 345 families received medication delivery through the pharmacy partner.
The result: the rate of primary care patients with well-controlled asthma improved from 48 percent to 54 percent.
COMMUNITY FOCUS ON SCHOOL-BASED SUPPORT
At the wider population level, the team identified a need for improved screening and communication. In response, the network worked to build a deeper relationship between Cincinnati Children’s, the Cincinnati Health Department, and the Cincinnati Public Schools, the county’s largest school system.
“School nurses were crucial,” says Mansour. The collaboration helped school nurses identify all students known to have asthma, conduct more asthma control screenings, and intervene in some cases before miscommunications or care disruptions escalated into serious asthma exacerbations.
THE WORK CONTINUES
Follow-up plans include using technology to further expand reach. A pilot project led by Theresa Guilbert, MD, MS, shows positive results from providing telemedicine services for children at school, as well as providing electronic inhaler monitors and medication bottles with digital caps for remote tracking.
Beyond technology, however, the co-authors say relationship building was the key to improved outcomes—and forging partnerships takes time.
“Would other communities do this exactly the same way?” Mansour says. “Perhaps not. But if you have leaders with the will, and partners with a shared vision, I do believe this approach is replicable.”
| Original title: | Association of an Asthma Improvement Collaborative With Health Care Utilization in Medicaid-Insured Pediatric Patients in an Urban Community. |
| Published in: | JAMA Pediatrics |
| Publish date: | Nov. 1, 2017 |
Research By