HLH Meets its Match: Persistence and Smart Medicine Just Might Outwit This Deadly Disorder
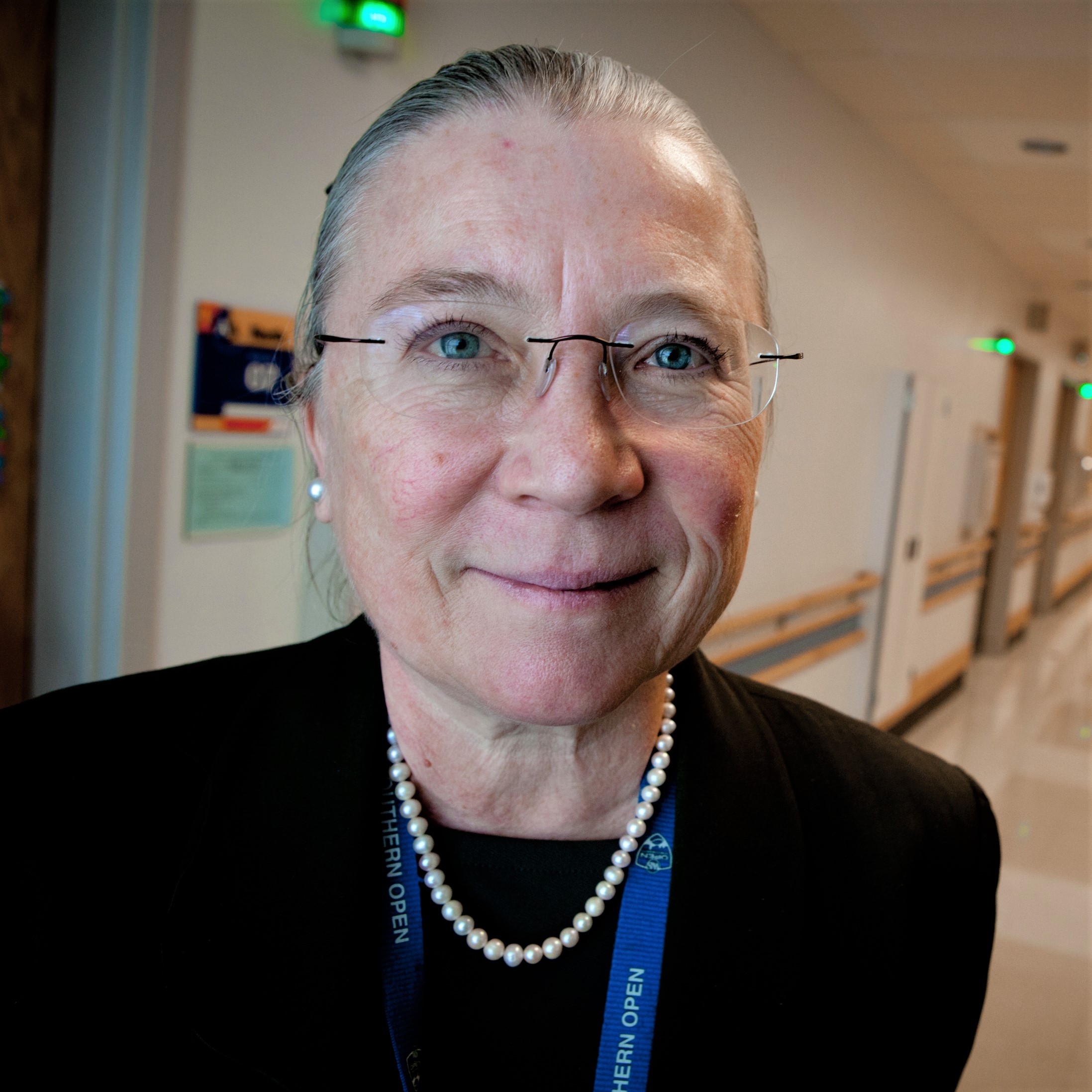
Research By: Lisa Filipovich, MD
Post Date: June 26, 2019 | Publish Date: January 2013

The child had a host of life-threatening complications: an enlarged liver and spleen, low blood count, inflammation in the brain. No one knew what it was, or what to do about it.
But Lisa Filipovich, MD, was certain of one thing. Figuring it out would be her life’s work.
It was some 30 years ago, Filipovich’s first day as a faculty member at the University of Minnesota Hospital. But she remembers it as if it were yesterday.
“It was one of the most fascinating and challenging areas of medicine I’d experienced. But it wasn’t anything we had learned in training. No one knew what it was. It hadn’t even been described in the medical literature.”
She knows now that “it” was hemophagocytic lymphohistiocytosis (HLH), a life-threatening immunodeficiency. For people with HLH, the body’s normal reaction to infection goes into overdrive, resulting in swelling, pain, and eventually, life-threatening damage to organs and systems throughout the body.
THE FIRST MAJOR STEP
Filipovich, now director of the Immune Deficiency and Histiocytosis Program at Cincinnati Children’s, and one of the world’s leading authorities on HLH, says a big breakthrough in understanding the disease came in the late ’90s, when the first genetic cause was identified. People who shared the disorder’s unique set of abnormalities had a common genetic mutation that kept them from producing perforin, a protein crucial to the function of the immune system.
“It began to explain why the natural killer cells and other cytolytic cells in this disease don’t work,” says Filipovich, “but it still didn’t tell us why patients got the disease.
The process of better understanding and managing HLH is one that has occupied Filipovich and her team for the last 20 years. And although it has not yet yielded a cure, it has certainly led to more successful treatment.
“We have built an extremely talented team with a strategy of providing treatment in safer, smarter ways.”
—Lisa Filipovich, MD
STEPS TOWARD PROGRESS AGAINST A RARE DISEASE
“There are two steps in treating this disease,” says Filipovich. “First is to stop the destructive inflammatory process. But many patients then need their immune system changed over with a bone marrow transplant.”
HLH has both inherited and acquired forms. It can occur at almost any age, although it most often strikes infants and young children, even babies in utero. It typically starts with an infection. In highly susceptible individuals, it can be triggered by a childhood immunization.
“At first, the immune system turns on as it should, to contend with whatever the infectious agent is,” explains Filipovich. “The problem is, it gets going and can’t turn off. That’s what leads to the toxicity, to the destruction of the blood cells.”
From there begins a downward spiral that can include liver failure, respiratory distress, inflammation in the brain and the inability to fight infection.
EARLY DETECTION IS KEY TO LIVING WITH HLH
Because HLH is considered a “rare” disease (statistics say it occurs in about one in a million children), many healthcare providers are unfamiliar with its symptoms, and it often goes undiagnosed for too long.
“One of the problems is, no one stumbles to the diagnosis soon enough,” Filipovich says. “And it’s the ‘soon enough’ that is the problem.”
To halt the rampant inflammation of HLH, doctors currently use high-dose steroids, but with a number of side effects. Filipovich and other members of her team (see story that follows) are working on studies to evaluate therapies with fewer toxic effects.
“It would be a great advance if the disease could be controlled with far less collateral damage,” she says.
ADVANCES IN BONE MARROW TRANSPLANTS REDUCE RISK
Once the inflammation is under control, most patients must have their immune systems replaced by means of a bone marrow transplant. The team at Cincinnati Children’s does more bone marrow transplants for HLH than any other center in the United States or Europe, with impressive results.
“We have made pivotal advances in this area,” Filipovich says. One of the advances is the use of “reduced intensity conditioning,” which uses a milder biologic agent to prepare a child for bone marrow transplant. The approach has far less systemic toxicity than the usual chemotherapy. It cannot be used for every child, says Filipovich, but for those who are eligible, it has improved long term survival to 90 percent.
What “long term” survival means for children with HLH is still to be determined, Filipovich says. She continues to follow patients that she treated more than a decade ago but acknowledges that there is a long way to go.
“We’re getting there,” Filipovich says. “But there are people who, for reasons we don’t understand, are far more fragile than others. Sometimes there are clues in the way they’ve responded to drugs or other things in the past. But we’re not yet smart enough to use that information to personalize their treatment.”
Even so, Filipovich and her colleagues have made an enormous difference for many children with HLH.
“We have built an extremely talented team with a strategy of providing treatment in safer, smarter ways,” she says. “In the old days, if a patient was in desperate situation, we would go right to transplant. But we’ve learned to move beyond desperation medicine. We have to do smart and calculated medicine. In the end, you have to move quickly but in a thoughtful way.”
Learn more about our work to defeat HLH.
—Story originally appeared in the Winter 2013 issue of Research Horizons.