Heart Institute Researchers Delve Into Kidney-Cardiac Connections
Post Date: May 23, 2023 | Publish Date:
At the basic science level, it has long been known that an acute injury to the kidney, or chronic kidney damage, can trigger a secondary cardiomyopathy that’s independent of blood pressure.
Jeffery Molkentin, PhD, led a team of researchers interested in discovering if it’s possible to eliminate that comorbidity. Their study, titled “Interleukin-33 Mediates Cardiomyopathy After Acute Kidney Injury by Signaling to Cardiomyocytes,” was recently published by Circulation.
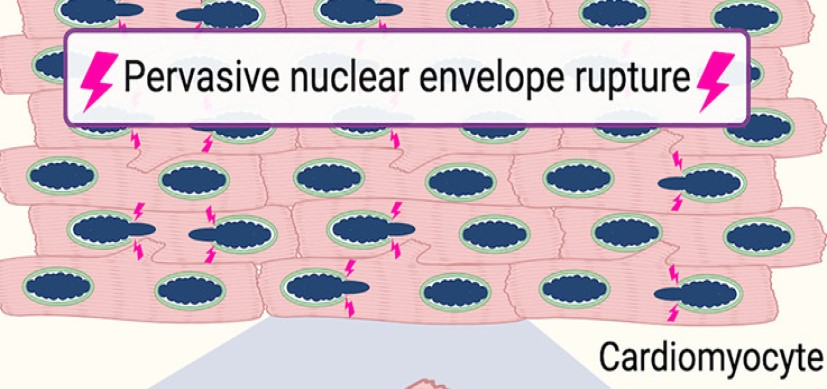
When the kidney is injured acutely, interleukin-33 (IL33) is released into the circulation causing cardiomyopathy. These researchers created mouse models with a deleted receptor gene for IL33 in the heart after AKI. They found that these mice are now protected from the cardiomyopathy that typically ensues after AKI.
They then created a mouse model that lacked the gene for IL33, and these mice were also protected from cardiomyopathy following AKI. Moreover, treating mice with a blocking antibody against IL33 was similarly protective to the heart after AKI.
“That’s exciting because IL33 monoclonal antibodies are in human clinical trials for other diseases already, which could mean a rapid translation to humans who are experiencing AKI or even chronic kidney disease,” says Molkentin, director of the Division of Molecular Cardiovascular Biology and executive co-director of the Heart Institute.
This research paves the path for development of a way to protect the human heart when the kidneys are starting to fail or when they have been injured acutely.
Learning to protect against postoperative acute kidney injury
Another study currently underway aims to decrease the amount of acute tubular necrosis (ATN) after cardiopulmonary bypass. ATN is a kidney disorder where damage to the tubule cells of the kidneys often causes acute kidney failure. Bypass causes inflammatory changes that can induce ATN.
This work is being led by Heart Institute leaders including David L.S. Morales, MD, executive co-director and director of cardiothoracic surgery, along with medical director and cardiologist David Cooper, MD, MPH, and nephrologist Stuart Goldstein, MD, who is director of the Center for Acute Care Nephrology.
Some reports in adults have shown that when inhaled nitric oxide is given through the cardiopulmonary bypass pump, it can decrease ATN. However, the exact mechanisms of how that occurs and the actual changes in the kidneys is unclear. In general, post-cardiopulmonary bypass renal failure and ATN are highly associated with increased mortality. The ultimate goal of this research is to help find a way to decrease that.
This research team created a sheep model and administered nitric oxide with cardiopulmonary bypass. They found evidence of a strong signal indicating nitric oxide decreased incidence of post-cardiopulmonary bypass ATN.
This work will serve as the foundation for conducting a formal multi-institutional study of the use of nitric oxide in children undergoing heart surgery that Cooper will be leading.
The researchers presented this work at the American Association for Thoracic Surgery’s annual meeting in May 2023.
Nephrology and Heart Institute faculty co-author multinational consensus statement
Cincinnati Children’s physicians were recently involved in co-authoring a consensus statement from the Acute Disease Quality Initiative (ADQI). It is the first time in ADQI’s history that a consensus statement focuses solely on acute kidney disease in children.
The statement, “Consensus-Based Recommendations on Priority Activities to Address Acute Kidney Injury in Children,” was published in JAMA Network Open.
The statement was developed by a panel of 47 international experts at the 26th Acute Disease Quality Initiative meeting held in November 2021. It includes consensus statements specific to acute kidney injury as it relates to epidemiology, diagnostics, mechanical support, educational goals, and biologic and physiologic development of the growing child. The panel also identified gaps in knowledge and areas for further research.
“For a pediatric consensus document to be published in a journal with such impact and worldwide reach is unprecedented,” says first author, Stuart Goldstein, MD. Further underlining the link between the kidneys and heart, Goldstein serves as both director of the Center for Acute Care Nephrology and co-director of the Heart Institute Research Core at Cincinnati Children’s. Katja Gist, DO, MSc, Cardiac Intensive Care Unit (CICU) physician and co-director of the Heart Institute’s Center for Acute Care Nephrology, was pediatric ADQI co-chair for the section on AKI biomarkers.
ADQI represents leading universities worldwide and sets new standards for the diagnosis and management of acute kidney injury and related disorders. The November 2021 ADQI was the group’s first devoted to children.