Compromised Skin Outweighs Inheritance as Allergy Risk
Research By: Jocelyn Biagini Myers, PhD
Post Date: February 18, 2020 | Publish Date: Feb. 5, 2020

“We found that children with atopic dermatitis were at higher risk of sensitization to both food and aeroallergens, suggesting that aeroallergens and foods find their way through the skin when the barrier is compromised.”
—Jocelyn Biagini Myers, PhD
When it comes to the risk a child faces of developing severe allergies, growing up with a compromised skin barrier appears to be even more significant than the genes inherited from a parent with allergies, according to new research from asthma and allergy experts at Cincinnati Children’s.
Detailed findings from comparing two groups of children, one with atopic dermatitis (AD)—often called eczema—and one at high risk of developing allergies and asthma, appear online in pre-proof format in the Journal of Allergy and Clinical Immunology. The study was led by first author John Kroner, MS, and senior author Jocelyn Biagini Myers, PhD. The work includes eight co-authors from Cincinnati Children’s and the University of Cincinnati.
The study compared data from children in two studies:
- Children with family histories of allergy and/or asthma who had been enrolled in the long-running Cincinnati Childhood Air Pollution Study (CCAAPS).
- And children with atopic dermatitis (AD) who had been enrolled in the ongoing Mechanisms of Progression of Atopic Dermatitis to Asthma in Children (MPAACH) study, the first pediatric cohort of AD in the United States.
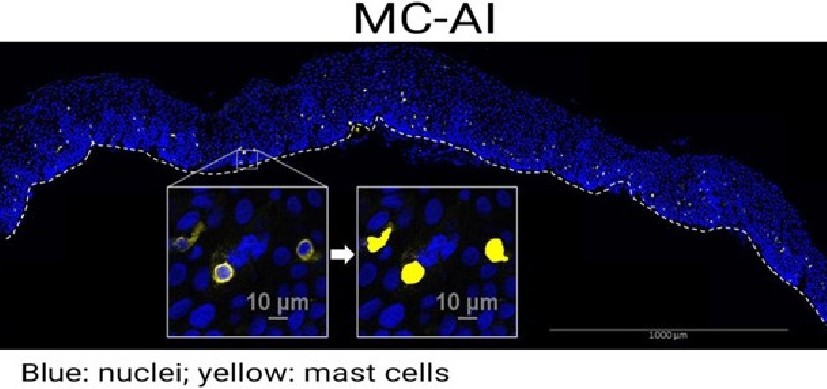
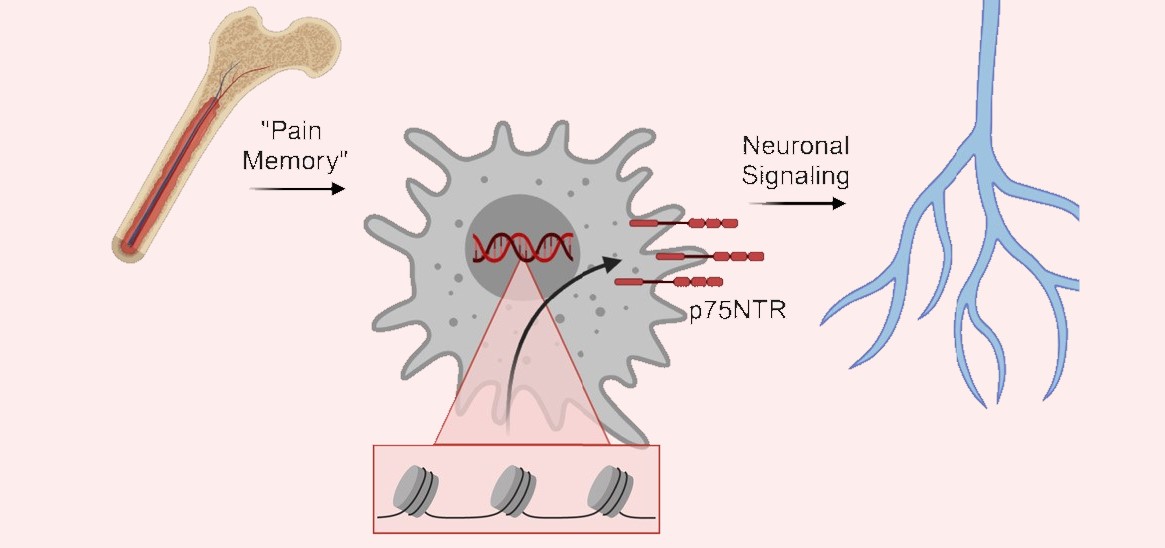
“We found that the rate of allergic sensitization was 1.5 fold higher in children with AD compared to those with only a parental history of allergic disease, supporting that AD increases risk over heredity alone,” Biagini Myers says. “Further, we found that children with AD were at higher risk of sensitization to both food and aeroallergens suggesting that aeroallergens and foods find their way through the skin when the barrier is compromised.”
When compared to the CCAAPS cohort, MPAACH children were significantly more likely to be sensitized to any allergen (42.2% vs 28.8%), and co-sensitized to both food and aeroallergens (14.8% vs 4.2%). The MPAACH children were also significantly more likely to be sensitized to dog (11.7% vs 1.4%), cockroach (5.5% vs 2.0%) and egg allergens (26.6% vs 12.3%) .
“Our findings strongly suggest that interventions aimed at improving the skin barrier in early childhood may help prevent allergic disease,” Biagini Myers says.
Approximately 10% of children in the U.S. develop atopic dermatitis—a skin inflammation associated with itchiness and rash. While the terms eczema and atopic dermatitis are often used interchangably, AD more specifically emphasizes damaged-skin conditions that carry allergy risk.
More research is needed to determine which groups of children have the highest need for skin protection interventions and what levels of protection they may need.
| Original title: | Atopic Dermatitis Independently Increases Sensitization above Parental Atopy: the MPAACH Study |
| Published in: | Journal of Allergy and Clinical Immunology |
| Publish date: | Feb. 5, 2020 |
Research By