Chorioamnionitis Directly Harms the Brains of Very Preterm Infants
Research By: Viral Jain, MD | Nehal Parikh, DO, MS
Post Date: June 2, 2022 | Publish Date: May 26, 2022
MRI-based study from CINEPS investigators reveals neurological effects independent of premature birth
A dangerous form of infection-related inflammation that can occur during pregnancy appears to directly cause brain injury among very preterm infants—those born between 22 and 32 weeks gestation.
The study, published online May 26, 2022, in the American Journal of Obstetrics and Gynecology, paper was published by members of the Cincinnati Infant Neurodevelopment Early Prediction Study (CINEPS) at Cincinnati Children’s.
CINEPS was launched in 2016 by neonatologist Nehal Parikh, DO, MS, and colleagues to identify early markers of neurodevelopmental disabilities such as cerebral palsy and cognitive deficits using advanced modes of brain MRI (magnetic resonance imaging) and sophisticated statistical modeling. The cohort involves more than 350 very preterm infants.
What is chorioamnionitis?
This serious complication, also known as intraamniotic infection, is commonly caused by a bacterial infection that can trigger dangerous tissue inflammation in the mother and fetus, preterm labor, and even very premature birth.
Chorioamnionitis occurs in about 4% of pregnancies that reach full term. However, it occurs in 25-40% of preterm deliveries.
Findings address lingering controversy
Many in the field have argued that any adverse effects on brain development associated with chorioamnionitis are the result of the premature birth itself.
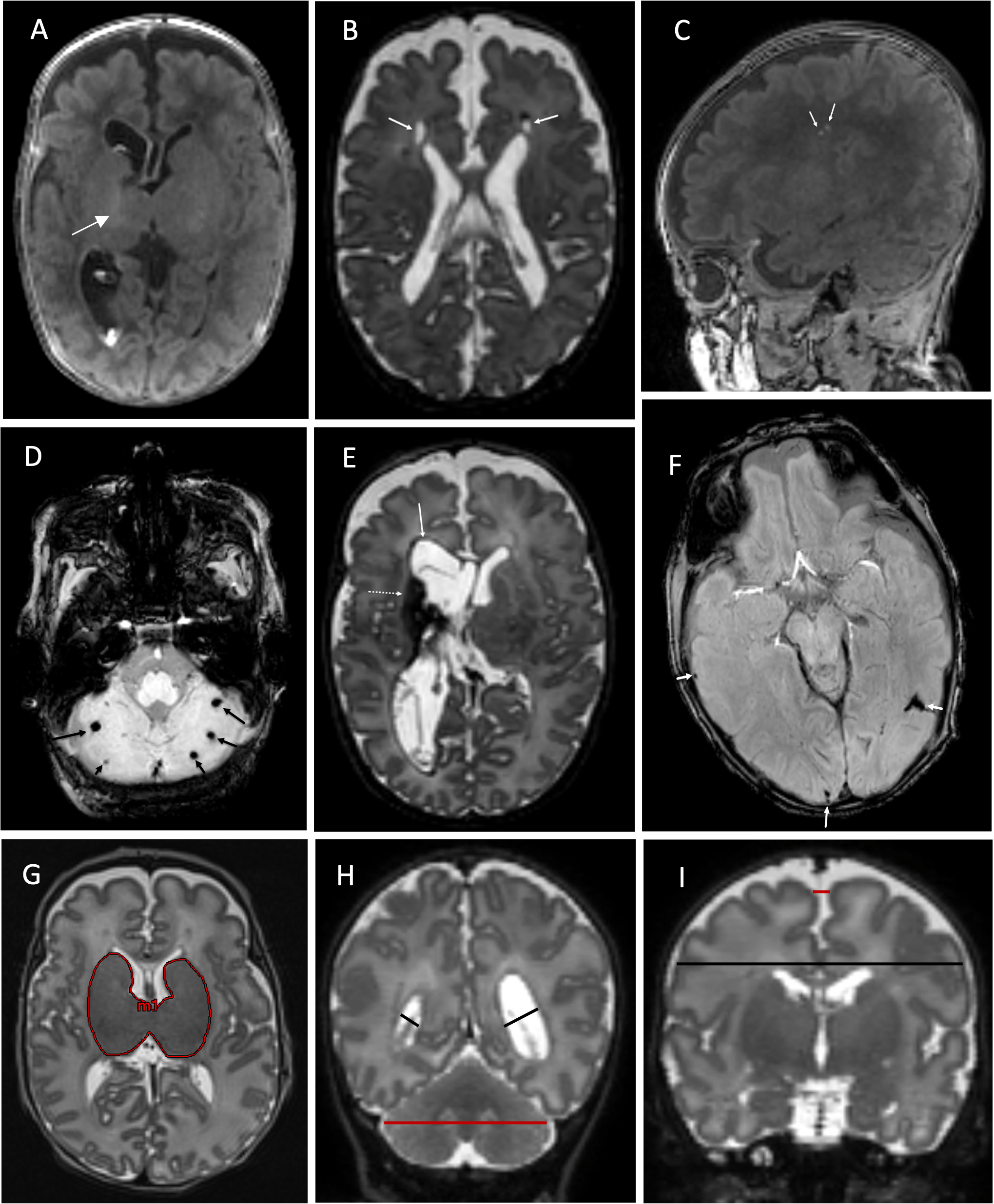
To test this, the CINEPS team examined MRI brain scans of 353 very preterm infants, 56 of whom had moderate to severe acute histological chorioamnionitis. They found that infants with at least moderate chorioamnionitis also had significantly higher brain abnormality scores than the control group.
“Mediation analyses demonstrated that 50% of brain abnormalities resulted indirectly from premature birth and the remaining 50% from a direct effect of moderate to severe acute histological chorioamnionitis as compared to preterm infants with no/mild chorioamnionitis,” the co-authors state.
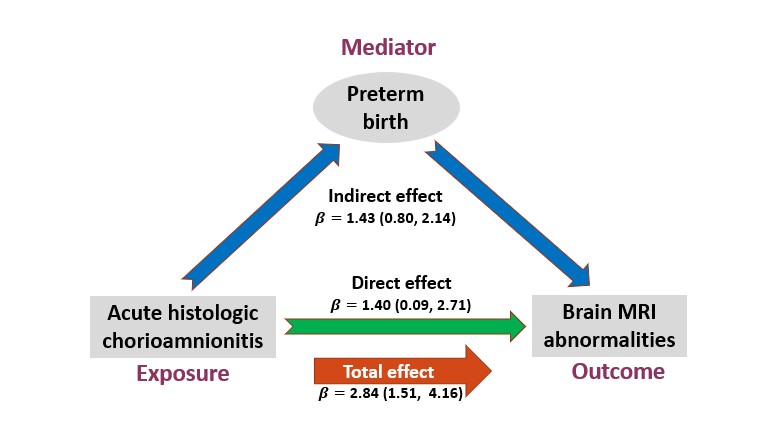
“This resolves a long-standing debate in the field and paves the way for early prevention trials (e.g., anti-inflammatory meds) while using brain MRI as a surrogate endpoint. Our findings may also influence obstetricians to identify and treat chorioamnionitis sooner to prevent its many downstream adverse effects,” says Parikh, senior author for the study and director of the Center for Prevention of Neurodevelopmental Disorders at Cincinnati Children’s.
Next steps
Earlier this year, researchers at Cincinnati Children’s published proof of principle findings (online March 30, 2022) in Science Translational Medicine that showed, in an animal model, that anti-inflammatory treatment can prevent lung damage related to chorioamnionitis.
One next step for researchers will be to explore whether anti-inflammatories also can reduce or prevent brain damage from the condition.
Another next step may be encouraging more consistent testing to detect infections.
“Because histologic chorioamnionitis can frequently present without clinical symptoms, the study findings may increase obstetric practice of testing amniotic fluid for infections in mothers with preterm labor and/or premature rupture of membranes,” Parikh says. “Targeted and earlier treatment with antibiotics could reduce the risk of neonatal complications.”
| Original title: | Acute histologic chorioamnionitis independently and directly increases the risk for brain abnormalities seen on MRI in very preterm infants |
| Published in: | American Journal of Obstetrics and Gynecology |
| Publish date: | May 26, 2022 |
Research By