Broad Immune Response to HIV Linked to Development of B Cells
Research By: Krishna Roskin, PhD
Post Date: January 22, 2020 | Publish Date: Jan. 20, 2020

When an individual is infected with human immunodeficiency virus (HIV), their immune system begins a game of cat-and-mouse—as the virus evolves, so does immunity. During this process, each individual’s immune system can react in different ways. What causes some to react more robustly than others?
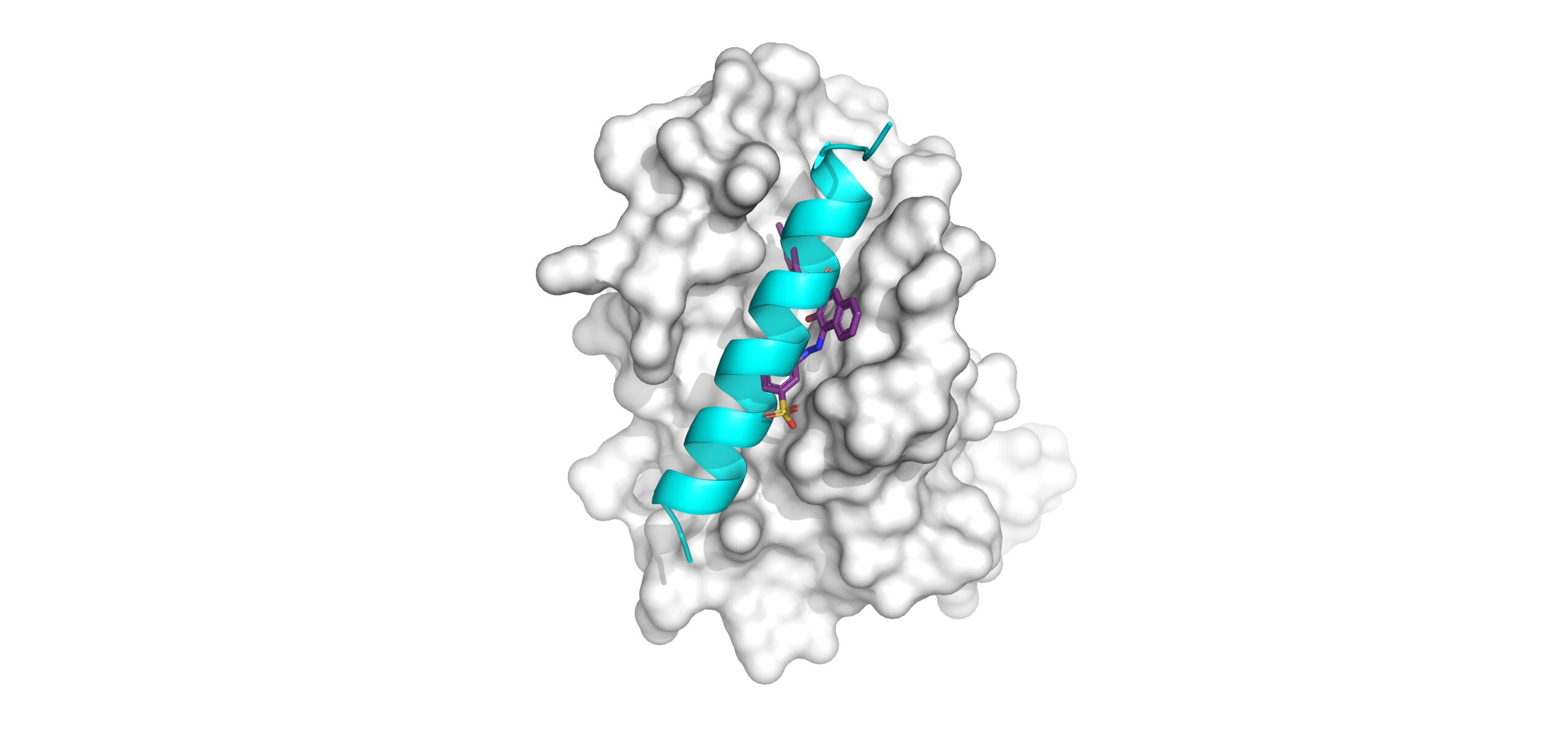
B cells could provide answers, according to a study published in Nature Immunology led by researchers at Cincinnati Children’s, Stanford University, and Duke University. The team sequenced antibodies genes from HIV-positive groups to determine why some develop broadly-neutralizing antibody (bNAb) responses while others do not. They discovered that bNAb subjects show systematic differences in B cell repertoire formation and selection.
What causes a bNAb response?
HIV bNAbs are antibodies that can defend cells from a broad range of HIV strains. After years of chronic infection, between 10 and 50 percent of HIV-infected individuals develop bNAb responses. If an individual is infected with just one strain of HIV, why do they sometimes develop these antibodies to fight off other strains?
“We know that people who make bNAbs tend to have more of the HIV virus,” says lead investigator Krishna Roskin, PhD, of the Division of Biomedical Informatics at Cincinnati Children’s. “It’s not that they have an easier battle, but it does seem like there’s something about their immune system that’s different.”
To explore this difference, researchers analyzed antibody heavy-chain gene repertoires from HIV-positive groups with bNAb, HIV-positive groups without bNAb (noNAb), and HIV-negative control groups. As they studied the library of B cells from each of these groups, patterns began to emerge.
The bNAb subjects each had hundreds to thousands of antibody lineages with long CDR-H3s, a region in the antibody chain that is critical for adaptive immune function. They also showed very high levels of somatic hypermutation, a process in which the immune system adapts its response to new threats. Conversely, the noNAb and HIV-negative subjects appeared to select against these traits.
How could bNAbs contribute to HIV vaccines?
Although there are just two main types of HIV, the virus branches out into many different strains—and researchers are continuously discovering more as HIV mutates and changes over time.
“There are so many strains of HIV, and it evolves so quickly, you never really know which version you may be exposed to,” Roskin says. “The concern is that if we vaccinate for one strain, there will always be another. A viable HIV vaccine needs to elicit broad protection.”
While bNAbs are not able to clear HIV in the people who make them, learning more about bNAbs and how they work is a priority for HIV vaccine development efforts. Coaxing the immune system to make bNAb-like antibodies as part of a vaccine response could potentially protect against a wide range of strains, making vaccines more effective.
“The challenge is that it takes years for HIV-positive individuals to develop this response, which is difficult to do with a vaccine,” Roskin says. “We want to take what we’ve learned about the immune systems of bNAb subjects and apply this to HIV-negative subjects. If we can get healthy people to make bNAbs, they can develop a broad immunoresponse to protect them.”
Visit the Roskin lab for more data-based immunology research.
Article written by Dakota Campbell, Division of Biomedical Informatics
| Original title: | Aberrant B cell repertoire selection associated with HIV neutralizing antibody breadth |
| Published in: | Nature Immunology |
| Publish date: | Jan. 20, 2020 |
Research By