Berwick: US Health System Still Too Focused on Being a ‘Repair Shop’
Post Date: June 2, 2021 | Publish Date:
Addressing deep health inequities requires deeper moral commitment to improving population health, says quality guru Don Berwick, MD
Despite vast sums spent on medical services, despite astounding technological advances, the United States remains mired with a fundamentally unfair health care system that still excludes far too many people.
We can do better at bridging gulfs in life expectancy and other disturbing inequities across racial, ethnic and gender groups, but getting there will require pharmaceutical companies, insurers, hospitals and government to stop “confiscating” funding that could be directed toward building a healthier society, says Donald Berwick, MD, a longtime leading voice in health systems improvement.
Berwick’s challenge to the medical establishment came June 1, 2021, in the third installment of the Cincinnati Children’s speaker series “Envisioning Our Future for Children.” Listen to previous speakers and register here for upcoming events.
Berwick’s career achievements include co-founding the Institute for Healthcare Improvement in 1989 and serving as Administrator of the Centers for Medicare and Medicaid Services (CMS) during the Obama administration.
US fares poorly in too many health measures
A number of well-known shortfalls in US health care have resurfaced in the wake of the COVID-19 pandemic and the social and political rifts widened in the aftermath of the murder of George Floyd in May 2020, Berwick said in an hour-long virtual discussion.
“We know what creates health and well being. It’s not the healthcare repair shop.” Berwick says. “There’s a strong relationship between government investments … and the actual conditions of the social determinants. In the US, we’ve gone backwards.”
Among his examples:
- A 50-year shift in tax rates favoring the well-to-do.
- A 10-year gap between rich and poor in life expectancy for US women at age 40; and a 15-year gap for men. Both of which are felt more acutely among minority populations.
- Evidence that adverse childhood experiences–far more common among Blacks and Latinos than whites–multiply the risks of 9 of the 10 leading causes of death in America, including heart disease, cancer, kidney disease, Alzheimer’s disease and suicide.
- Glaring racial differences in the Child Opportunity Index.
What are the social determinants of health?
Berwick recapped six factors that define a healthy population, noting that none of them are especially new.
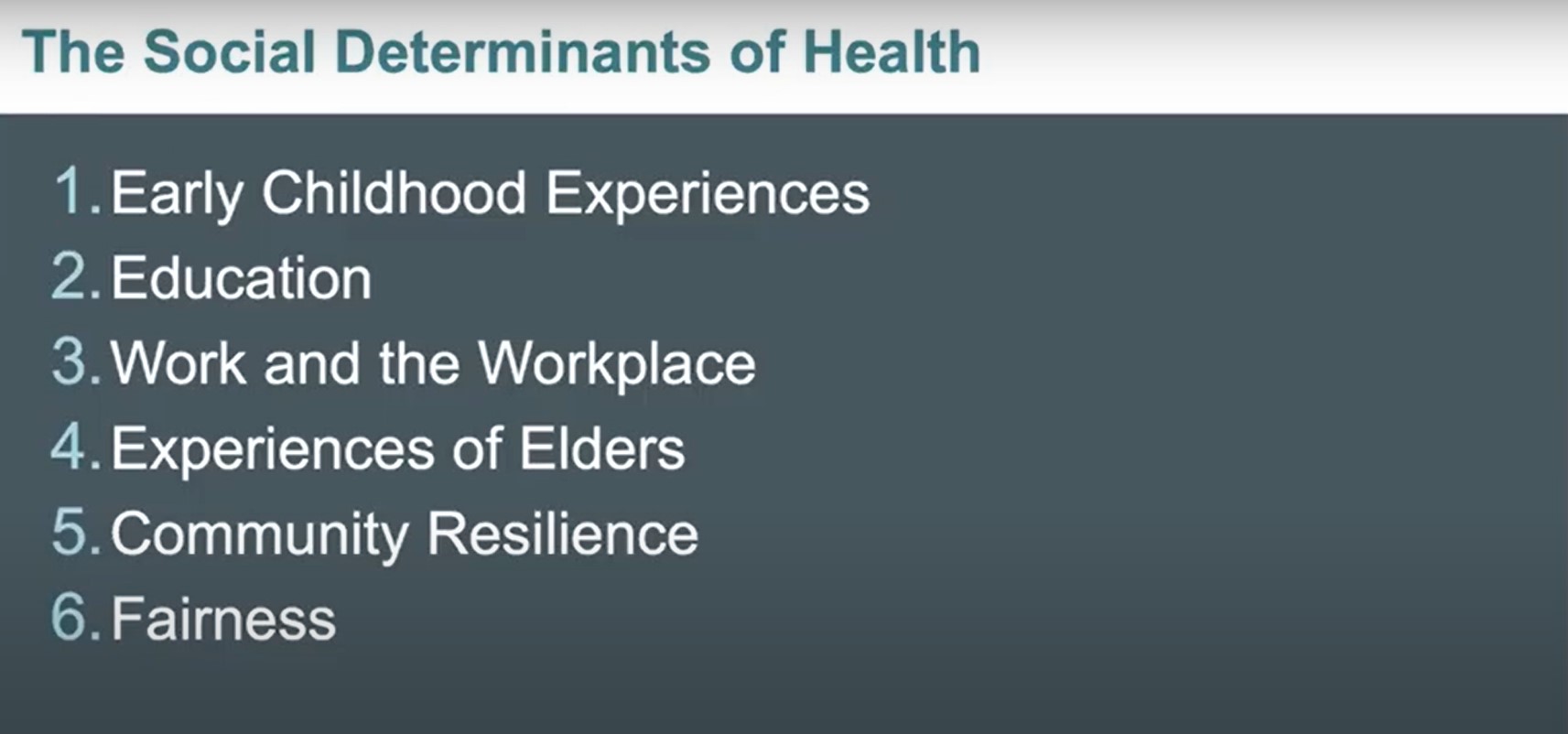
The problem has been a lack of commitment, especially to issues of fairness. Countries with an ethos of fairness built into their public policies spend about $2 on social wellness investments for every dollar spent on health services. But the US spends about 90 cents on social supports for every dollar spent on health care, Berwick says.
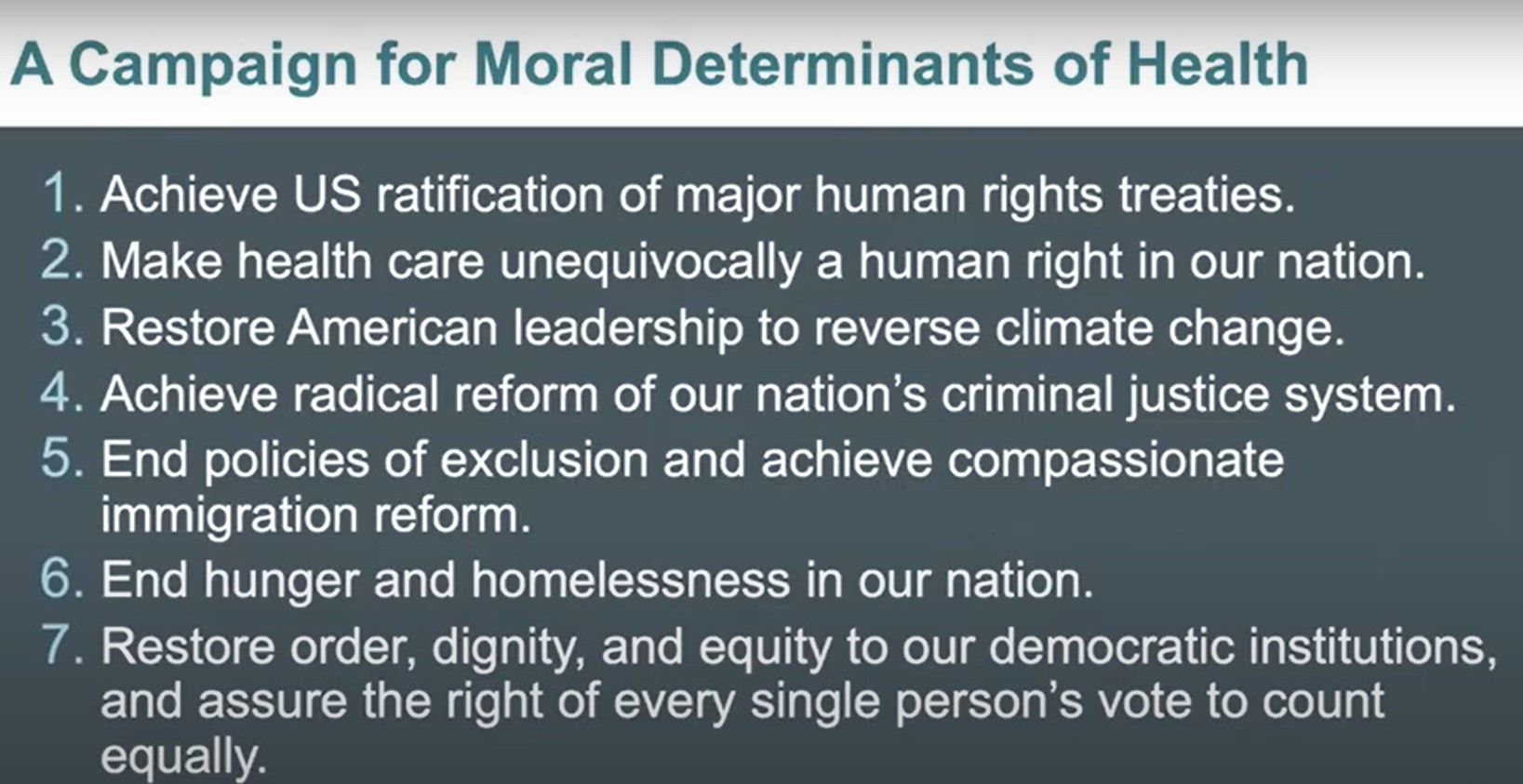
What are the moral determinants of health?
Achieving true health improvement across populations in America requires going beyond gaining an understanding of the social factors at work. It requires influential organizations to take moral stances that drive action. These are seven topics Berwick advocates about:
How can hospitals help
Berwick praises Cincinnati Children’s as a long-time leader in many aspects of healthcare quality improvement. In fact, he has interacted with leaders here for many years, going back to 2002 when Cincinnati Children’s became one of 13 organizations to join the Pursuing Perfection initiative launched by the Robert Woods Johnson Foundation.
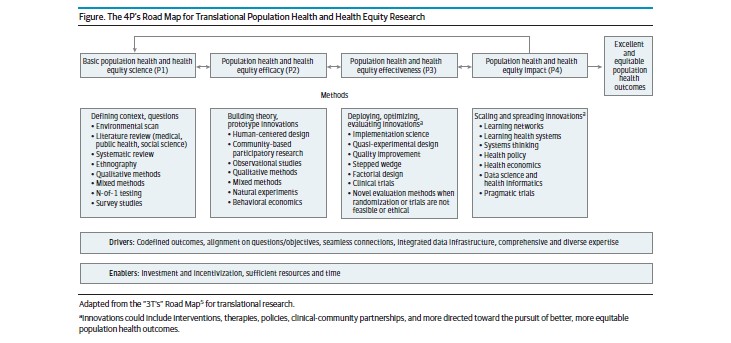
That work ultimately led to the formation of the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s, which was built under the leadership of Uma Kotagal, MD, and now led by co-directors Peter Margolis, MD, PhD, and Steve Muething, MD.
Now, hospital leaders need to demonstrate even deeper commitments to improving population health, Berwick says. He recommends that hospitals pick one or more of the moral issues he advocates to focus upon as part of an overall broadening and re-thinking of their missions.
Hospitals can become much more active participants in issues such as reducing hunger, eliminating homelessness, or addressing the population-scale health problems worsened by America’s criminal justice system, Berwick says.
One of the first steps to achieving such goals: the health care “repair” system needs to stop constantly asking for more money, be it setting excessive drug prices or charging ever-higher fees for services.
“Health care confiscates much more than it needs,” Berwick says. “And that includes Cincinnati.”
The health care sector and the wider corporate business world share a mutual responsibility that goes beyond achieving short-term profits.
“What kind of society do you want?” Berwick asks. “And what’s your role in creating it?”
Recommended reading
Berwick says “The Health Gap,” written in 2015 by Michael Marmot, should be mandatory reading for people in health care.
The new Child Opportunity Index can be viewed in more detail here.
Coming up
Register now to hear Aviv Regev, PhD, Executive Vice President, Genentech Research and Early Development, who will speak at 2 pm July 29 about the topic “Design for Inference.”
Read more about research at Cincinnati Children’s addressing health inequities