A Study That Changed the Direction of Cardiac Stem Cell Research
Post Date: June 27, 2019 | Publish Date: January 2015
Top Research Achievements 2010-2015
Since 2010, scientists at Cincinnati Children’s have produced more than 7,000 peer-reviewed studies with far-reaching impact across pediatric medicine. From this impressive body of work, six advances stand out as Cincinnati Children’s premier scientific achievements of 2010-15.
Sometimes great medicine boils down to figuring out why an exciting new treatment approach just does not work. This is how Jeffery Molkentin, PhD, rocked the world of cardiac research in 2014. From the instant scientists discovered how to create stem cells that did not require the use of embryonic tissue, experiments began to find a way to use stem cells to regenerate the human heart.
Few missions in medicine have had higher priority. Heart disease is the nation’s leading cause of death. Beyond the fatalities, the damage caused by sudden heart attacks and gradual heart failure destroys the quality of life for millions of people while incurring hundreds of billions in health care costs. And yet, despite massive demand for cures, deep investment in research, and great expectations for stem cell technology, cardiac muscle remains stubbornly resistant to repair.
For several years, it seemed that regenerative medicine was poised for a breakthrough. Excitement ran high for the possibility that cardiac progenitor cells or even bone marrow cells expressing the cell surface protein c-kit could be injected into damaged or dead areas of the heart to directly create new beating tissue.
However, what was reported to work so well in mice and rats produced dismal results in human clinical trials in more than 4,000 patients worldwide. Molkentin’s team explained why in a paper published May 7, 2014, in Nature.
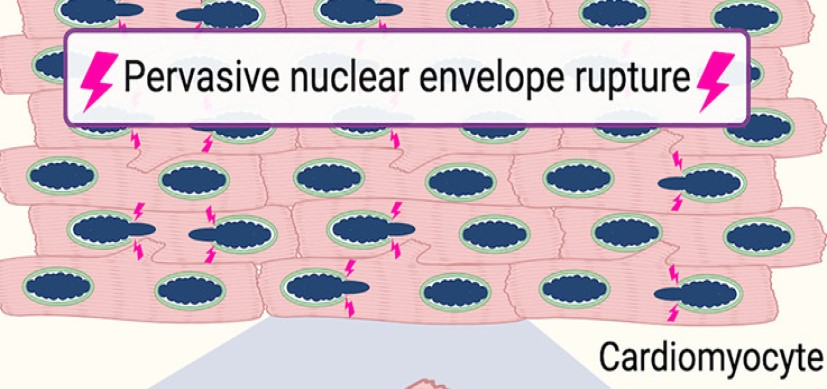
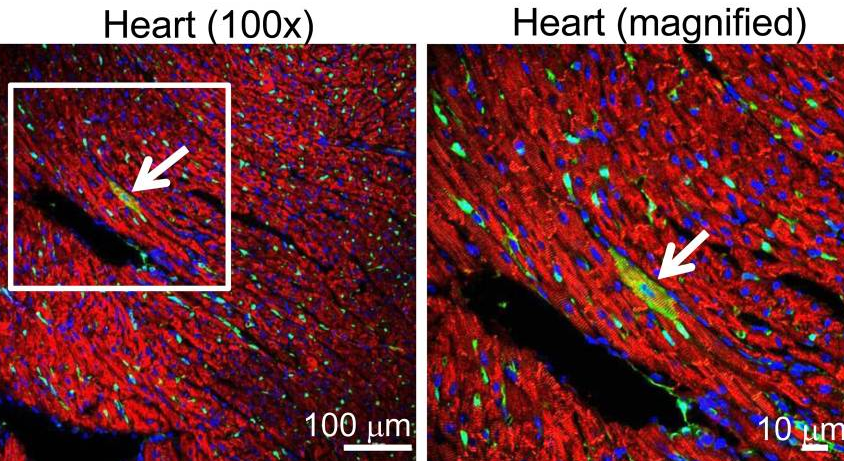
In this study, Molkentin’s team developed a genetic strategy in mice so that any new myocyte arising from a potential c-kit stem cell would be labeled green with a fluorescent protein. The lack of color told the story; just 0.027 percent of the murine cardiomyocytes originated from c-kit stem cells. To the extent that c-kit stem cells offered any therapeutic benefit, it was through small improvements to blood vessels, not generation of new muscle tissue.
“What we showed in our study is that c-kit-positive stem cells from the heart can make endothelial cells that form capillaries. But these c-kit positive cells do not like to make cardiomyocytes,” Molkentin says. “If they really do generate new cardiomyocytes, the rates are exceptionally low – roughly one in every 3,000 cells – and that becomes meaningless.”
These findings shocked the field and stirred extensive scientific debate. Ultimately, Molkentin’s work helped reprioritize how future clinical trials are planned, or no longer planned, and freed the research community to begin looking in new directions for a regenerative therapy that can work as intended.
Visit the Molkentin Lab
(This story originally appeared in the 2015 Research Annual Report)